Sinus Tarsi Syndrome
(AKA: Sinus Tarsi Impingement)
Summary
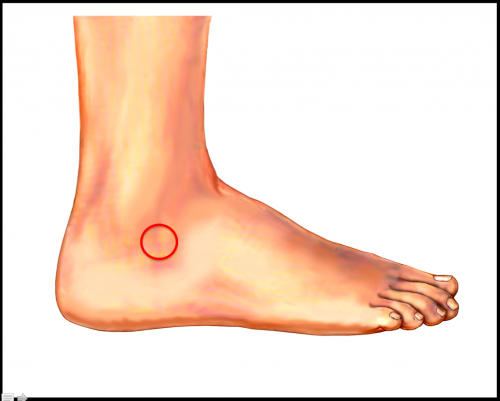
Sinus tarsi syndrome or sinus tarsi impingement is characterized by acute, localized pain in the outside front part of the ankle (sinus tarsi). Physical examination will localize pain and swelling to this area (Figure 1). Symptoms are often exacerbated by standing and walking, and there may be an associated flatfoot deformity. Treatment is oriented towards modifying activities, wearing comfortable shoes, trying ankle bracing, and possibly getting a local injection of corticosteroids. All of these treatments are designed to improve symptoms. Occasionally, surgery may be contemplated for a recalcitrant sinus tarsi syndrome. However if surgery is considered, it needs to address the specific cause of sinus tarsi syndrome.
Sinus Tarsi Impingement Summary Handout
Clinical Presentation of Sinus Tarsi Impingement
Patients with sinus tarsi syndrome present with pain in the front and outside of the ankle (anterolateral ankle). Symptoms are often aggravated by standing or walking. Pain may be quite localized. The pain can develop slowly over time, or it may be precipitated by a period of increased activity. It is important to rule out other specific causes of pain in this area of the ankle (peroneal tendinitis, anterior process fracture of the calcaneus, tarsal coalition, stress fractures, etc.)
Physical Examination of Sinus Tarsi impingement
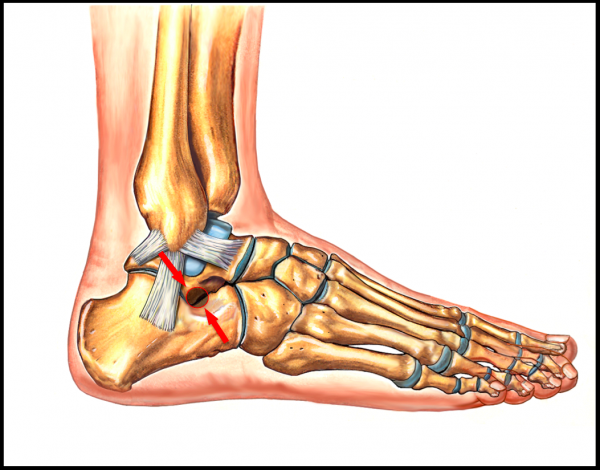
Physical examination will identify localized pain just in front of and below the prominent bone (fibula) on the outside of the ankle (Figure 2). There may be associated swelling in this area. Rotating the foot to the outside may reproduce symptoms. A flatfoot may be a prominent feature of this condition.
Imaging Studies
X-rays may show some impingement in the sinus tarsi area. This can show up as an increased density of bone right where the lower bone of the ankle (talus) jams into the heel bone (calcaneus). X-rays are also helpful to rule out other causes of pain in the anterolateral aspect of the ankle (ex. calcaneal process fracture).
An MRI or CT scan is usually not needed unless surgery is being contemplated. When performed an MRI often shows evidence of increased blood flow (edema) in the involved bones (calcaneus, talus and fibula). An MRI may also show fluid and inflammation associated with the sinus tarsi, where the outside lower (anterior and posterior) aspect of the talus impinges on the heel bone (calcaneus) in the sinus tarsi. In some patients cysts in the heel bone (calcaneus) will be noted right at the level of the impingement with the talus. An MRI may reveal possible etiology behind the pain, such as fibrous coalition or abnormal connection between two bones, or a stress fracture in the bones in the vicinity such as the talus.
Treatment
Non-Operative Treatment
Treatment is usually non-operative. It consists of:
- Activity modification: Avoiding activities that precipitate symptoms.
- Comfort Shoewear: Symptoms can be improved with the use of comfortable shoes consisting of a shock absorbing heel, a relatively stiff sole, and a rocker contour to help disperse the force more evenly up the leg.
- Heel lift or Elevated Heel: A heel rise of 8-12mm (where the heel is higher than the forefoot) can serve to limit how much the heel bone needs to move on the bone above it (the talus) thereby serving to decrease the exteent of sinus tarsi impingement. Conversely, the use of flat soled shoes or bare feet may serve to exacerbate the symptoms of sinus tarsi impingement.
- Ankle Lacer: An ankle brace may be helpful to limit and minimize symptoms.
- Anti-inflammatory medications (NSAIDs): Pain and swelling may be improved with the use of anti-inflammatory medications, provided there is no contra-indications to taking this type of medication.
- Corticosteroid injection: A local injection of corticosteroids into the sinus tarsi may help settle symptoms in this area.
Operative Treatment
Surgical treatment may be considered for patients that have truly failed non-operative treatment. However, it needs to be contemplated with care as sinus tarsi syndrome is often a final manifestation of another more integrated problem, such as an acquired adult flatfoot deformity. In the setting of a flatfoot, the foot essentially slides off of the lower bone of the ankle and impinges on the outside. Therefore, sinus tarsi syndrome in this setting requires not just a cleaning out of the sinus tarsi (debridement), but perhaps a reconstruction of the foot or a subtalar fusion.
Edited by Stephen Pinney MD, August 31st 2025. Previously Edited by Vinod Panchbhavi MD, and Dave Townshend, MD