Charcot-Marie Tooth Disease Foot Deformities (CMT)
Summary
Charcot-Marie Tooth (CMT) disease is a condition that commonly produces a high arched foot (Figure 1). It was described independently by Jean-Martin Charcot, Pierre Marie, and Howard Henry Tooth in 1886. It is also known as Hereditary Sensorimotor Neuropathy (HSMN), or Peroneal Muscular Atrophy. CMT is associated with weakness of the many lower extremity muscles. It is caused by abnormalities in nerve conduction (too much myelin in the nerve sheath). CMT is usually inherited, and therefore a positive family history is common – although up to a quarter of the cases can arise spontaneously. The foot deformities and symptoms related to CMT are typically progressive – they tend to worsen over time. However, the rate at which they worsen can vary greatly. Some patients are able to function at a high level throughout their lives (mild cases), whereas some develop debilitating foot (and sometimes hand) symptoms relatively early (severe cases).
Figure 1: Typical Charcot-Marie-Tooth Foot Deformity

Clinical Presentation
The clinical manifestations of CMT can vary widely. The most common complaints are those associated with high arched feet, loose ankles, and muscle weakness. These include a higher chance of suffering:
- Recurrent ankle sprains
- Ankle instability
- Fractures of the 5th Metatarsal – outside border of the boot
- Peroneal tendonitis
- Sesamoiditis – pain at the small bone under the big toe
- Drop foot (in more severe cases)
- Ankle arthritis (later in life)
- Claw toe deformities
It is not uncommon to have noticeable clawing of the toes (including the big toe) in patients with CMT.
Physical Examination
Muscle testing may reveal muscle weakness. Commonly, the ability to bring the foot inwards (inversion) is stronger that the ability to move the foot outward (eversion). Also, the ability to push the foot down (plantar flexion) is stronger than the ability to lift the foot up (dorsiflexion).There is a classic set of muscle imbalances that leads to the common Charcot-Marie-Tooth foot deformities. These four muscle imbalances include:
- The Peroneus Brevis (outside ankle) is weaker than the Tibialis Posterior muscle (inside of ankle). This leads to a greater inward pull of the foot (inversion).
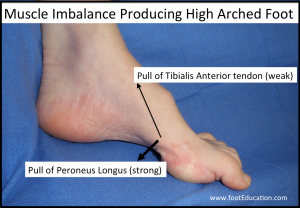
- The Tibialis anterior muscle is weaker than the Peroneus Longus muscle. This creates the high arch by pulling the front of the foot down (Figure 2).
- The intrinsic foot muscles (the small muscles in the sole of the foot that help move the toes) are weaker than the extrinsic muscles (the larger muscles in the lower leg that cross the ankle joint and help move the toes). This muscle imbalance leads to clawing of the toes, including the great toe.
- The Anterior compartment muscles (the muscles at the front of the shin bone or tibia) are weaker than the calf muscles. This can lead to a drop foot.
Skin sensation of the foot (the ability to feel things) can sometimes be affected in more severe cases.
Figure 2: The unopposed pull of the peroneus longus causes the classic deformity of Charcot-Marie Tooth disease. This creates the high arch by pulling the forefoot down.
Imaging Studies
Weight-bearing x-rays of the foot and ankle will show evidence of a high arched foot pattern. Classically, the heel bone will have an elevated angle relative to the ground and the 1st metatarsal bone (the bone the big toe is attached to) will be pointed down (Figure 3).
Figure 3: Typical Charcot-Marie-Tooth Foot X-rays


Treatment
Treatment of CMT has focused on helping the symptoms created by the deformity. To date, no treatment has been shown to fix the actual underlying nerve problem. If the foot and ankle joints are flexible, with minimal arthritis, it is more likely that the procedures recommended will aim to rebalance and realign the foot, while preserving motion. This usually involves lengthening or moving tendons and cutting and realigning bones in the foot. If the foot and ankle are stiff, or if there is arthritis in the joints, it is more likely that the procedures recommended will aim to fuse the joints in a better position.
Non-Operative Treatment
Non-operative treatment focuses on controlling/correcting the foot deformities, maintaining muscle strength, preventing ankle sprains, and controlling pain symptoms. Treatments often include:
- Ankle Lacer: This can be an effective brace to help hold the ankle stable, and may improve ankle symptoms in patients with mild to moderate foot
- Ankle-Foot-Orthotic (AFO): An AFO can be used to improve symptoms in patients with more pronounced deformities or more extensive hindfoot arthritis, by supporting the foot and holding it very stable.
- Orthotic insert: A shoe insert with a low spot under the big toe and/or raised area under the outside of the heel and midfoot, can help to reposition the foot in patients who still have some flexibility.
- Physical Therapy: Physical Therapy to improve muscle strength and proprioception (the ability of your brain to understand where your ankle is in space relative to your body) can help protect against future ankle sprains, and serve to improve overall function.
- For patients with tendonitis or arthritis symptoms, anti-inflammatory medications (NSAIDs), can help to decrease pain and improve their overall function
Operative Treatment
Operative treatment is often performed to help correct the foot deformity. It is important to understand that the foot deformities occur because of the muscle imbalances that affect the foot, so it may be necessary to transfer tendons (and their muscles) to help rebalance the foot. Surgery for Charcot-Marie-Tooth foot deformities must be individualized for each patient based on their deformity, their muscle function, and their age. Often, a combination of procedures are needed and are often performed at the same time. Common surgical procedures used to address Charcot-Marie-Tooth foot deformities include:
- Peroneus Longus to Peroneus Brevis tendon transfer
- Release of the tight ligaments on the inside of the foot (talonavicular joint capsule release)
- Release of the tight plantar fascia
- Lengthening of the Achilles Tendon
- Repositioning the 1st metatarsal bone (dorsiflexing 1st metatarsal osteotomy)
- Cutting the heel bone and shifting it to the outside (Lateralizing calcaneal osteotomy)
- Claw toe correction
- Jones procedure to correct a clawed hallux (clawed big toe)
- Peroneal tendon debridement or repair
- Lateral ankle ligament stabilization
- Drop foot correction (Tibialis posterior transfer to the dorsal foot)
- Ankle debridement – Removing painful bone spurs from the ankle
- Ankle fusion
Edited by Stephen Pinney MD, October 9th 2025. previously edited by Anthony Van Bergeyk and Haley Merrill, MD.