Superficial Peroneal Neuritis
Summary
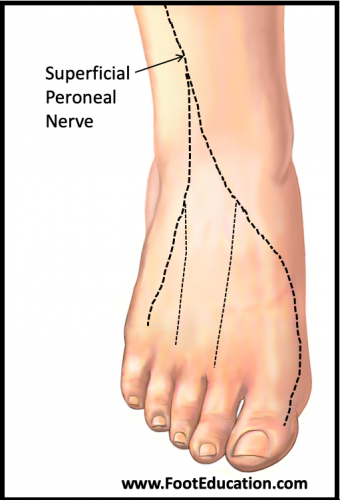
Superficial peroneal neuritis occurs as a result of injury, scarring, inflammation, or direct pressure of the superficial peroneal nerve, also referred to as the superficial fibular nerve. The superficial peroneal nerve (Figure 1) branches from the common peroneal nerve at about the level of the knee, descends along the outer (lateral) side of the front of the ankle, then splits into two branches just above the level of the ankle. This nerve provides sensation to the outer (lateral) sides of the lower leg and the top of the foot. Superficial peroneal neuritis can be caused by direct or indirect trauma to the outer side of the lower leg or ankle (ex. blunt force to the leg, fibular fracture, ankle fracture, or following arthroscopic ankle surgery). This neuritis can also be caused by compression of the nerve at any point along its path. Patients will present with numbness, pain, or tingling. The location of these symptoms helps determine the specific site of the injury. Treatment of superficial peroneal neuritis varies based on the underlying cause of injury. Treatment can include NSAIDs, removal of triggers, physical therapy to break up scar tissue, or surgery.
Figure 1: Superficial Peroneal Nerve
Clinical Presentation
Patients with superficial peroneal neuritis often will present with a history of one the following risk factors:
- Trauma to the outer side of the leg or ankle
- Recent surgery in the area surrounding the nerve
- Behaviors that frequently compress the path of the nerve
- Tumor that may compress the path of the nerve (rare)
Patients typically present with numbness, tingling, or pain across the top (dorsum) of the foot. They commonly have a history of a direct trauma or surgery (ex. ankle fracture repair or ankle arthroscopy) that can lead to an injury or scarring that involves the superficial peroneal nerve. If the trauma that causes neuritis is an injury that occurs closer to the knee joint (more proximally) the pain may be distributed across a broader area -and in some situations there may even be loss of muscle function leading to a footdrop. In some patients’ direct pressure over the area of the superficial nerve such as tightly applied shin pads or a walker boot that is too tight will lead to the neuritic symptoms.
In a small percentage of patients who develop a superficial peroneal neuritis the nerve firings resulting from the injured area of the nerve will cause other nerves in the lower leg to fire excessively and become overly sensitive. This is due to a reflex arch via the low back (lumbar spine chord) and can lead to a painful complex regional pain syndrome.
Physical Examination
The goal of the physical examination in patients in whom a superficial peroneal neuritis is suspected is to: identify the area of the nerve that has been injured or affected; and determine the effect that the neuritis has had (ex. loss of sensation and/or loss of muscle function). To help determine the area of the nerve that has been injured or affected the clinician will look for a Tinel’s sign. This involves tapping along the path of the nerve to localize the site of nerve injury or entrapment. This test is considered positive if the tapping elicits local pain or discomfort and a tingling sensation that radiates towards the top of the foot. Physical examination may also reveal weakness of the muscles supporting the outside of the ankle. The two peroneal muscles (Peroneus Longus and Peroneus Brevis) help stabilize the outside of the ankle and are innervated by the superficial peroneal nerve so an injury to this nerve near the outside of the knee could lead to weakness or loss of function of these muscles.
Imaging
X-ray and CT can be used to assess any associated bony injury, such as fractures and bone fragments.
MRI and Ultrasound can identify soft tissue abnormalities, such as bone spurs or tumors causing compression of the nerve.
Nerve Conduction Studies and Electromyography (EMG)
In some patients with a superficial peroneal neuritis a nerve conduction test or EMG may be ordered. A nerve conduction study can be used to help determine if there is an abnormal flow/signal along a certain nerve course. An electromyography is used to determine whether a certain nerve is adequately innervating the muscles that it would normally innervate.
Treatment
Treatment of superficial peroneal neuritis is dependent on the type of injury or problem that has caused the neuritis. Treatment should targets the underlying cause of the neuritis. A common treatment is to simply remove the cause of the neuritis. If a shin pad or tight walker boot is constricting the leg or ankle and causing a superficial peroneal neuritis removing this constriction should lead to resolution of symptoms over time. However, if the neuritis is a result of a traumatic or surgical injury that leads to scarring around the nerve more involved treatment may be required. Physical therapy including focused soft-tissue/scar massage can be helpful to breakup adhesions that have formed around the nerve. Physical therapy may also be helpful in treating weakness of the leg or ankle in certain patients. NSAIDs to decrease the inflammation can also be helpful in decreasing symptoms caused by superficial peroneal tendonitis. In some patients the treating physician may prescribe other medications such as gabapentin to help stabilize the nerve firings and decrease the associated symptoms.
Surgical Treatment of Superficial Peroneal Tendonitis
Operative measures include freeing up the scar tissue around the nerve (surgical decompression of the nerve) and excisions of any bone spurs, ganglions, or growths causing nerve compression. In patients where there has been a significant injury to the nerve leading to debilitating pain along the course of the nerve it may be necessary to cut the nerve (neurectomy) before the area of the injury which will lead to numbness over the top of the foot but can lessen the nerve pain symptoms considerably.
Edited June 15th, 2020