Ankle Fracture (Broken Ankle)
Summary
Ankle fractures are relatively common injuries. These injuries can vary greatly in severity. Many ankle fractures are not displaced and will heal well with time. Whereas other ankle fractures are notably displaced and require major surgery to realign the fractures. Severe ankle fractures may lead to ankle arthritis in some patients.
Ankle Fracture Overview
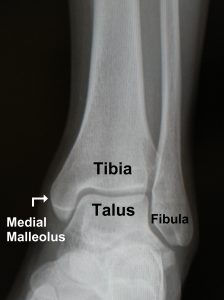
To understand ankle fractures it is helpful to understand ankle anatomy. The ankle joint is formed by three bones (Figure 1):
- The Tibia is the large bone of the lower leg that forms the top and inside (media and posterior malleolus) of the ankle joint.
- The Fibula is the smaller bone of the lower leg that makes up the outside (lateral malleolus) of the ankle joint.
- The Talus is the dome-shaped lower bone of the ankle that moves up and down within the joint.
An “ankle fracture” (broken ankle) occurs when one or both of the bones (fibula or tibia) making up the top part of the ankle joint are broken.
Ankle fractures can be broadly divided into two groups:
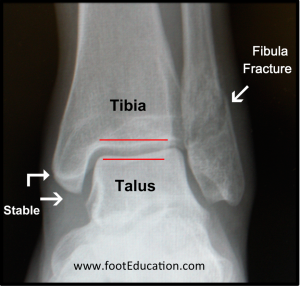
- Stable Ankle Fractures: The ankle joint remains intact (Figure 2)
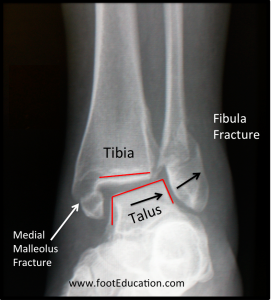
- Unstable Ankle Fractures: The ankle joint is displaced (Figure 3)
Ankle injuries routinely fall into predictable patterns based on how they happen. Understanding the mechanism of injury helps doctors to treat ankle fractures.
Most ankle fractures occur following an acute twisting injury when the foot is planted on the ground and the body rotates around i. When the foot rotates outward, the bone on the outside of the ankle (the fibula), breaks first. If the rotation continues, the structures on the inside of the ankle, the medial malleolus or the deltoid ligament will break or tear.
If the foot rotates inward, either the ligaments stabilizing the outside of the ankle will tear (sprain) or the medial malleolus will break first, followed by a fracture of the fibula as the rotation continues.
Sometimes a twisting injury will tear the strong fibrous tissue that holds the fibula and tibia together at the ankle (the syndesmosis) which can lead to a fibula fracture closer to the knee.
For successful treatment of an ankle fracture, it is very important for the ankle to be well aligned. If the ankle fracture heals with even 1 mm of shifting out of place, the result can be the development of ankle arthritis, with pain and stiffness of the joint.
A stable ankle fracture (Figure 2) occurs when the broken bones and ligament damage is mild enough that the ankle does not displace even with weight bearing. This can occur if the fractures are lower than the joint surface or sometimes when only the outside bone (fibula) or outside bone (tibia) is broken and the ligaments that stabilize the ankle are undamaged. Stable ankle fractures commoon and are most often treated non-operatively by limiting twisting stress to the ankle joint until the bones heal (typically 6 weeks). Sometimes stability is hard to assess initially. A cast or walking boot is typically applied and the patient is allowed to bear weight on the injured leg as tolerated. The Orthopaedic Surgeon will ask the patient to return in less than 10 days to see if the fracture displaces. If it does, it is unstable. If not, non-operative treatment can continue.
An unstable ankle fracture (Figure 3) occurs when the injury has disrupted the containment of the talus and it shifts, either to the side or to the front or back. This usually happens when there is injury to more than one bone or ligament of the ankle. Unstable ankle fractures typically benefit from surgery to realign the ankle joint and hold it in place while it heals (Figure 4). While ankle fracture surgery has risks, the risks of arthritis or failure to heal the bones without surgery is usually much higher.
Following an ankle fracture, some patients heal and return to full function without a problem. Unfortunately, even with ideal treatment, some patients with unstable ankle fractures may develop ankle arthritis as a result of the severity of the joint damage.

Edited on December 14th, 2023
Previously edited by Daniel Charlick MD, Lance Silverman MD, Timothy Charlton MD and John Early MD
sp/12.14.23