Achilles Tendon Rupture
Patient Handout: Achilles Tendon Ruptures
Summary
Achilles tendon ruptures commonly occur in athletic individuals in their 30s, 40s, and early 50s. However, there is also a small group of patients in their 70s and 80s who suffer this injury. The injury usually occurs after a sudden application of force resulting in rupture of the Achilles tendon. The diagnosis of an acute Achilles tendon rupture is made on clinical examination as x-rays will reveal the ankle bones to be normal. The Achilles is the largest and strongest tendon in the body. It is subject to 2-3 times body weight during normal walking and 3-6 times body weight or more with running and jumping activities. Regaining normal Achilles tendon function is important to resuming an active, healthy lifestyle. Achilles tendon ruptures can be successfully treated non-operatively, or operatively. Recent studies suggest that non-surgical and surgical treatment of Achilles tendon ruptures produce equivalent results in certain populations. Patients treated surgically can expect a more rapid return to a pre-injury level of activity and a lower rate of re-rupture. However, surgery poses risks of complications such as infection or wound healing problems. For this reason, non-operative treatment may be preferable in many individuals, especially those patients with diabetes, vascular disease, and those who are long-term smokers.
Clinical Presentation
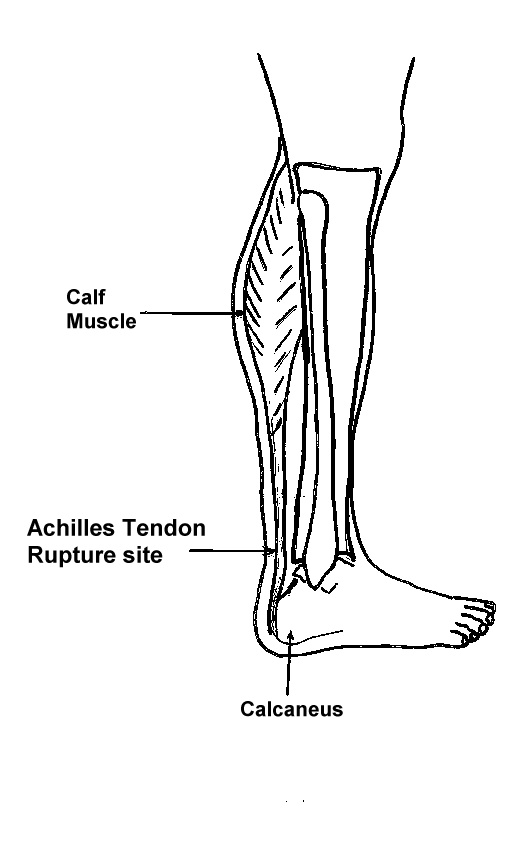
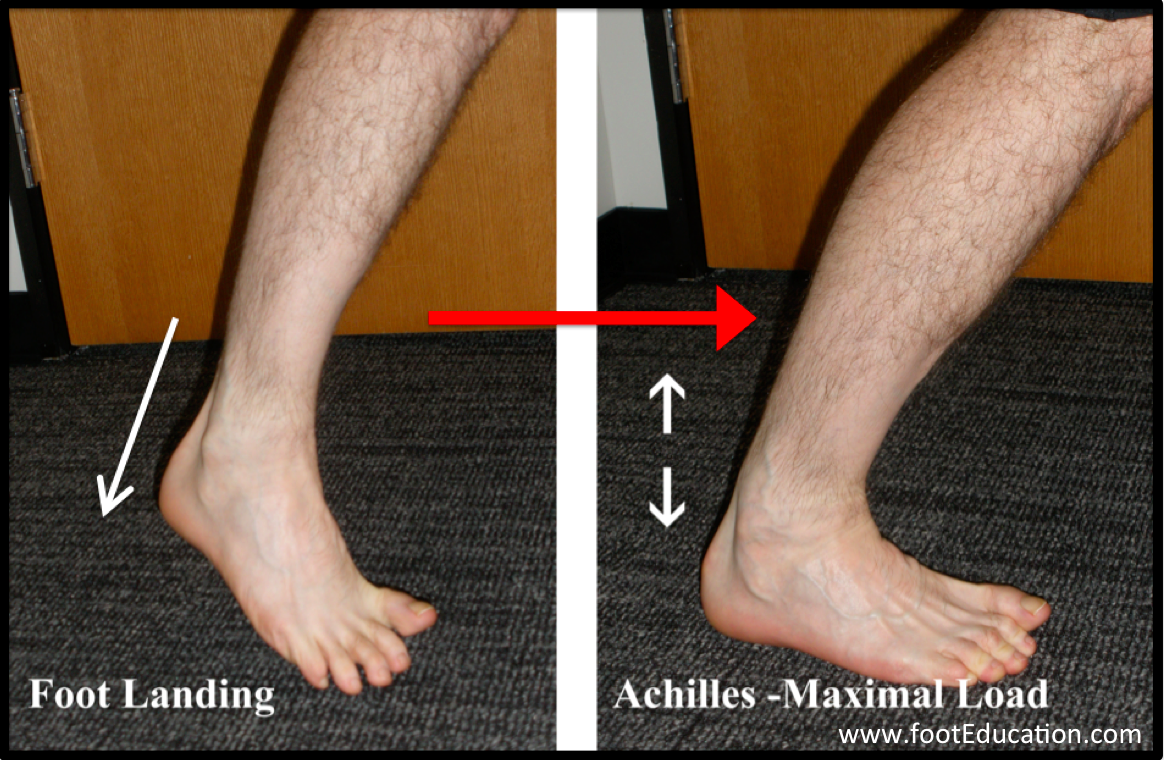
The Achilles tendon is the largest and strongest tendon in the body (Figure 1). It functions to transfer “push-off” force from the calf muscles to the heel bone. This force can be 2 to 6 times the body’s weight for activities such as walking, running, and jumping. Rupture of the Achilles tendon commonly occurs in individuals in their 30s, 40s, and early 50s but, no age group is immune. The underlying issue is that over time the Achilles tendon tends to become gradually weaker and stiffer as the body’s ability to repair is overcome by the repetitive injuries that may be associated with activity. Rupture of the tendon usually occurs when an athlete excessively loads the Achilles tendon usually in preparation to pushing off. Maximal load through the Achilles tendon occurs when the calf muscle is contracting while simultaneously the ankle is moving upwards (dorsiflexing) producing a lengthening of the tendon (eccentric loading). This can occur when changing directions, starting to run, stopping abruptly, jumping, or landing from a jump, (Figure 2). This sudden increased force through the tendon can lead to a rupture in the same way that a stretched rubber band may rupture. Individuals will feel a sharp intense pain in the back of their leg. Depending on the activity, individuals will often describe feeling as though they were “hit in the back of the leg” with a ball, a bat, or kicked. The rupture of the tendon can be extremely painful. The injury is associated with a fair amount of swelling and later, discoloration. Immediately following the injury, the pain varies a great deal. Some describe very little or no pain while others describe less but, persistent discomfort. While some individuals may be able to walk it is usually difficult. It is very rare that a rupture of the Achilles is partial. However, a painful Achilles tendonitis or a partial rupture of the calf muscle (gastrocnemius) as it inserts into the Achilles can also cause pain in this area. Examination by an experienced orthopaedic foot and ankle surgeon may be necessary to confirm the diagnosis.
Physical Examination
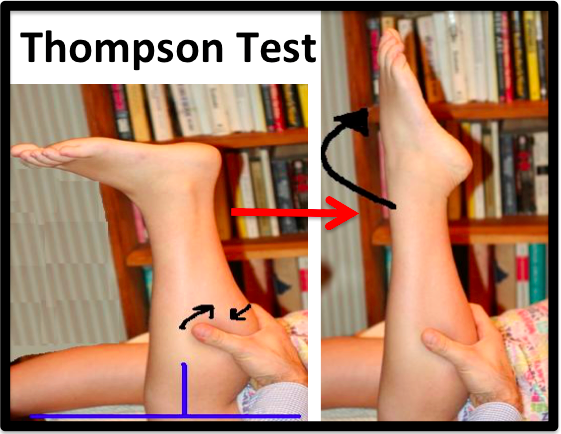
The diagnosis of an Achilles tendon rupture is made entirely on physical examination. Usually, there is a defect in the Achilles tendon at the site of the rupture that can be felt by lightly palpating the area. However, the main test is to determine whether the Achilles has been ruptured is the Thompson test (Figure 3). This essentially involves placing the patient on their stomach and squeezing the calf muscle. If the Achilles is intact, the foot will rise [plantar flex]. If it is ruptured, the foot will not move and will tend to be in a lower lying position.
Some patients mistakenly believe the tendon is working if they can push the foot down. However, patients will usually be able to move the foot up and down while sitting by using the muscles that move the foot side to side and flex the toes. Trying to push up while standing and applying body weight to the foot will reveal the true weakness. It will be difficult or impossible for a patient to stand on their toes for any length of time if they have suffered an Achilles tendon rupture -this is called the STAMP test. Sensation and circulation are not usually affected by an Achilles tendon rupture.
Imaging Studies
Plain x-rays may show an irregular appearance of the shadow that represents the Achilles on a side view (lateral view). However, more commonly plain x-rays are normal as the injury is to the tendon and therefore does not affect the bones of the foot. The rupture can be seen on ultrasound or MRI, but these studies are not necessary for acute, straight-forward injuries. Imaging with ultrasound and MRI is usually more helpful in the case of partial ruptures, tendonitis, or chronic Achilles conditions.
Treatment of Achilles Ruptures
Achilles tendon ruptures can be treated non-operatively or operatively. Both of these treatment approaches have advantages and disadvantages. Recent studies suggest that non-surgical and surgical treatment of Achilles tendon ruptures may produce equivalent results in many patients. However, the decision of how an Achilles tendon rupture should be treated needs to be based on each individual patient after the advantages and disadvantages of both treatment options have been reviewed. It is important to realize that while Achilles tendon ruptures can be treated either non-operatively or operatively, the injury MUST be treated. A neglected Achilles tendon rupture (i.e. one where the tendon ends are not kept opposed) will lead to chronic weakness, a notable limp, and often secondary problems with the knee, ankle and foot. Furthermore, trying to treat the problems associated with a neglected Achilles tendon rupture can be far more difficult than timely treatment of the original injury.
Non-Operative Treatment of Achilles Ruptures
Non-operative treatment of an Achilles tendon rupture consists of placing the foot in a toes-downward position [equinus] and immobilizing the foot in this position until the Achilles has healed. This typically involves some type of Cam Walker with a heel lift or a cast. A more aggressive rehabilitation program for patients undergoing non-operative treatment allows for graduated weight-bearing and controlled downward motion of the foot in the early phase of the recovery. However, it is often 6 weeks before full weight bearing in a boot or brace is allowed. In general, newer rehabilitation protocols allow for earlier movement of the healing tendon while protecting it from significant loads that would cause the healing tendon to disrupt or stretch out. It is very important that the status of the Achilles is monitored throughout non-operative treatment. This can be done by physical examination or via ultrasound. If there is evidence of gapping or non-healing, surgery may need to be considered.
Formal protocols have been developed to help optimize non-operative treatments and excellent results have been reported with these protocols. The focus of these treatments is to ensure that the Achilles rupture is in continuity and is healing in a satisfactory manner while at the same time preserving the function of the calf muscle by allowing some early motion.
The primary advantage of non-operative treatment is that without an incision in this area, there are no problems with wound healing or infection. Wound infection following Achilles tendon surgery can be a devastating complication and therefore, for many patients, especially those patients with diabetes, vascular disease, and patients who are smokers, non-operative treatment should be considered.
The main disadvantage of non-operative treatment is that the recovery is a bit slower. Consideration must be given to the overall effect of long-term immobilization and the deviation form “normal” activity for each individual patient. Surgical treatment may allow weight bearing in a Cam walker at 2-3 weeks after surgery. In addition, the re-rupture rate appears to be higher with non-operative treatments.
Operative Treatment of Achilles Tendon Ruptures
Operative treatment of Achilles tendon ruptures involves making an incision centered over the tendon rupture. The tendon is then repaired using sutures in such a way that the tendon ends are touching and tension is shared by the suture itself. This can be performed through a standard Achilles tendon repair technique or through a mini-incision technique. The minimally invasive technique of repairing the Achilles rupture has been shown to be equivalent in strength, but with fewer wound and infection complications than the standard open technique, albeit with a higher risk of nerve injury. Surgical repair allows for earlier weight bearing, joint motion, and lower leg muscle strengthening. Formal rehabilitation is important to the restoration of strength and balance. This can be achieved with the help of a supervised rehabilitation program – successful recovery from an Achilles tendon rupture is an active process over a number of months. Following surgical reconstruction, one may expect a full recovery by 8 to 12 months.
The potential advantages of surgical repair of the Achilles tendon include:
- Faster recovery: Return to pre-injury activities is faster with surgical treatment.
- Early Range of Motion: Patients are able to move the ankle earlier so it is easier to regain motion and strength and the rehabilitation program can be more aggressive.
- Lower Re-rupture Rate: The re-rupture rate may be significantly lower in operatively treated patients (2-5%) compared to patients treated non-operatively (8-12%).
The main disadvantage of surgical repair of the Achilles tendon rupture is the potential for a wound-healing problem, deep infection, or a painful scar.
Rehabilitation of Achilles Tendon Ruptures
Click here for a summary handout on Achilles Tendon Ruptures
Previously Edited by David Garras, MD, Michael Castro, MD, and Tim Charlton, MD
Edited on October 29th, 2024