Achilles Tendonitis – Non insertional
(Classic Achilles Tendonitis)
Summary
Achilles tendonitis is characterized by pain and swelling in the large tendon at the back of the heel (the Achilles tendon). Classic Achilles tendonitis is also called Non-Insertional Achilles tendonitis. This is because pain associated with Achilles tendonitis is located in the rope like part of the Achilles tendon. Whereas, in patients with insertional Achilles tendonitis the pain and swelling is in the area where the tendon inserts into the heel bone. Symptoms are often associated with an increase in activity level and tends to occur in patients in their 30s and 40s. Risk factors include increasing age, change in activity level, diabetes, and obesity. Treatment is usually non-operative and includes an initial period where the symptoms are allowed to settle, followed by a gradual return to activity. Treatment includes: avoiding aggravating activities; a shoe with a heel or a slight heel lift inside the shoe to off-load the tendon; anti-inflammatory medications (if tolerated); and exercises designed to both stretch and strengthen the Achilles tendon.
Achilles Tendonitis Summary Handout
Printable handout (complete webpage)
Clinical Presentation
There are three common causes for pain in the region near the back part of the heel:
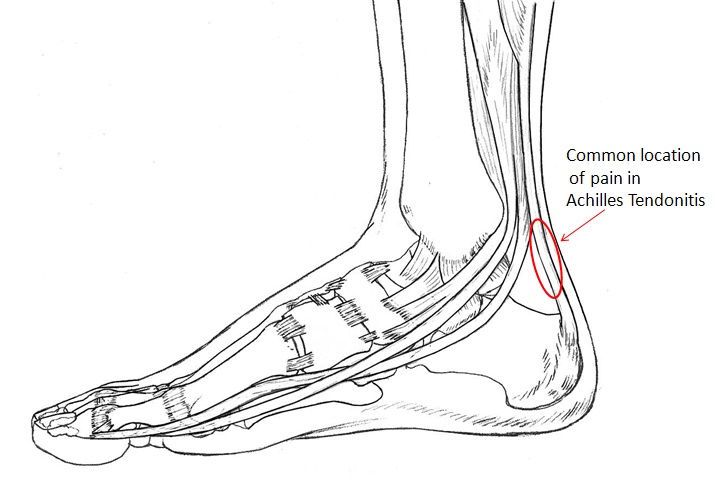
- Non-insertional Achilles tendonitis (Classic Achilles tendonitis): In classic Achilles tendonitis symptoms of pain and swelling are typically located 2-6cm above the insertion of the Achilles tendon to the heel bone. In some patients the pain may actually be from a thickening of the sheath surrounding the tendon (paratenonitis) rather than the tendon itself.
- Insertional Achilles tendonitis: In this type, the pathology is located at the insertion of the Achilles tendon to the heel bone.
- Achilles tendon rupture: Rupture of the Achilles tendon, usually 2-6cm from the insertion to the heel bone, while this condition usually occurs as an acute injury in some patients it may not be clinically obvious and can occasionally be confused with tendonitis
Achilles tendonitis is a chronic condition characterized by pain and often swelling in the Achilles tendon. Symptoms are occasionally due to swelling and inflammation of the tissue (paratenon) that surrounds the Achilles tendon – this is more accurately called tenosynovitis (Inflammation of the lining surrounding the Achilles tendon). Non-insertional tendinosis of the tendon often presents as an oblong lump in the tendon itself due to internal damage and microscopic tearing of the collagen fibers in the middle of the tendon. The location of the symptoms in non-insertional tendonitis is usually between 2-6 cm above the insertion of the Achilles tendon on to the heel bone (Figure 1). For Insertional Achilles Tendonitis, pain and swelling is located where the Achilles tendon inserts to the heel bone (Figure 1).

Achilles tendonitis is often associated with an increase in activity level such as starting a new training program or attempting to resume a normal activity level after an injury to another part of the foot or ankle. The use of shoes with “negative” heels as a way to “tone” the calf muscles has resulted in more Achilles tendonitis as these shoes tend to increase the load through the Achilles tendon. Irritation to the synovial sheath that encloses the Achilles tendon is thought to be caused either by direct pressure from shoe wear or from an irregularity in the Achilles tendon. The Achilles tendon is believed to suffer microtearing when it is overloaded, and the body’s healing response to this microtearing may also contribute to symptoms. Despite the pain originating from the Achilles tendon, the tendon itself is usually intact, and the presence of Achilles tendonitis is not believed to increase the risk of an Achilles Tendon rupture.
Physical Examination
Examination will usually reveal swelling and tenderness around the Achilles tendon (Figure 2). The physician may detect swollen, inflamed tissue lining the Achilles. If there has been any kind of an associated injury, it is important to ensure that the tendon is intact and that the problem is not, in fact, an Achilles tendon rupture. This is done by performing the “Thompson Test”, whereby the patient lies face down with their feet hanging off the end of the bed. The calf muscle is then squeezed and the foot should move if the Achilles is intact.
Imaging Studies
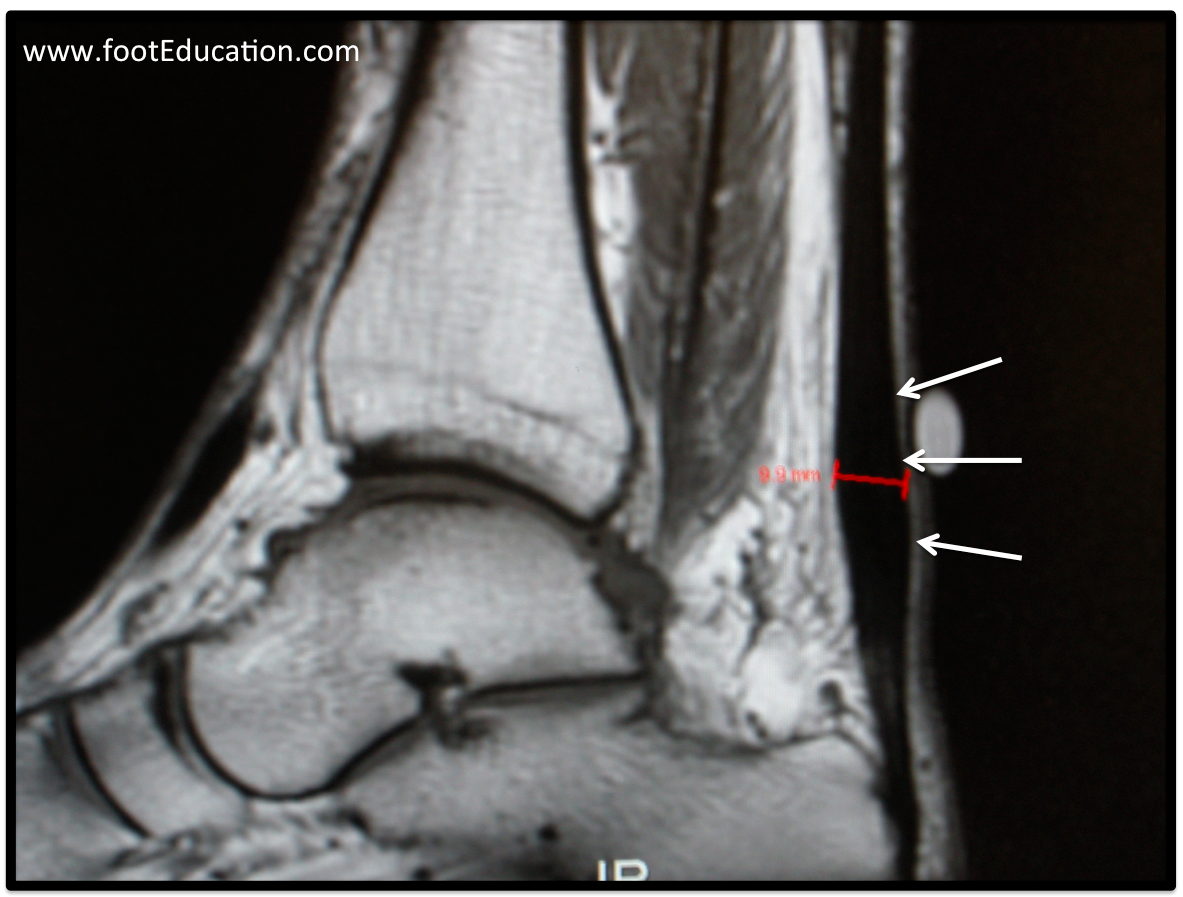
X-rays will usually be negative for non-insertional Achilles tendonitis, unless there is calcification of the Achilles tendon, which is relatively rare except in older patients. However, for insertional Achilles tendonitis, a calcaneal spur can be seen in an x-ray. An MRI can give a detailed view of the soft tissue (Figure 3) but is usually not indicated for an initial assessment of Achilles tendonitis, unless the physician is attempting to answer a specific question (i.e. is the tendon ruptured?). If needed an ultrasound can also be used as it is more readily available and less expensive than an MRI.
Treatment of Achilles Tendonitis: Non-Operative Treatment
Most patients with Achilles tendonitis can be treated effectively with non-operative treatment. This usually involves a period to let the symptoms settle, followed by a gradual return to normal activities. The elements of non-operative treatment may include:
- Activity Modification. In the short term, it may be necessary to stop any precipitating activities. Precipitating activities include high impact exercises that cause weight to be placed on the front part of the foot. This includes running, jumping, walking up hills and repetitive stair climbing. New training programs should be reviewed and stopped, at least until the symptoms resolve.
- Shoe Wear Modification. It is important to avoid shoes that precipitate or aggravate symptoms. In general, using well fitted “comfort” shoes will be beneficial. Some shoe modifications may also be helpful. Some patients will feel more comfortable in shoes with a slight heel, or with the addition of a heel lift inside the shoe. An increased heel height will tend to take some of the load off of the Achilles tendon. Patients should avoid shoes with a “Negative Heel” (i.e. the heel height is lower than the forefoot height) as this has been shown to increase the force through the Achilles, often leading to the development of Achilles tendonitis. Aggravating shoes should be modified or discarded so that they do not cause an increase or recurrence of symptoms.
- Medications. Non-Steroidal Anti-inflammatory medications, or NSAIDs, taken 1-3 times per day can help to settle symptoms in the short term, and break the cycle of pain and discomfort. However, for successful long-term management, NSAIDs usually need to be combined with other non-operative treatment strategies.
- Calf and Achilles Stretching. A tight calf muscle will increase the force going through the Achilles tendon and predispose the tendon to micro-tearing. A consistent calf stretching program is an important part of treatment. (Figure 4)

- Double leg heel rises. A high repetition, low resistance calf strengthening program can be very helpful in stretching and strengthening the Achilles tendon and calf muscle. Double leg heel rises, done in a controlled manner and performed while standing on the edge of stairs, (to allow for more movement through the ankle) can be very helpful. Consider starting with 5 sets of 5 repetitions and slowly over a period of weeks advance to 10-15 sets of 15 repetitions.
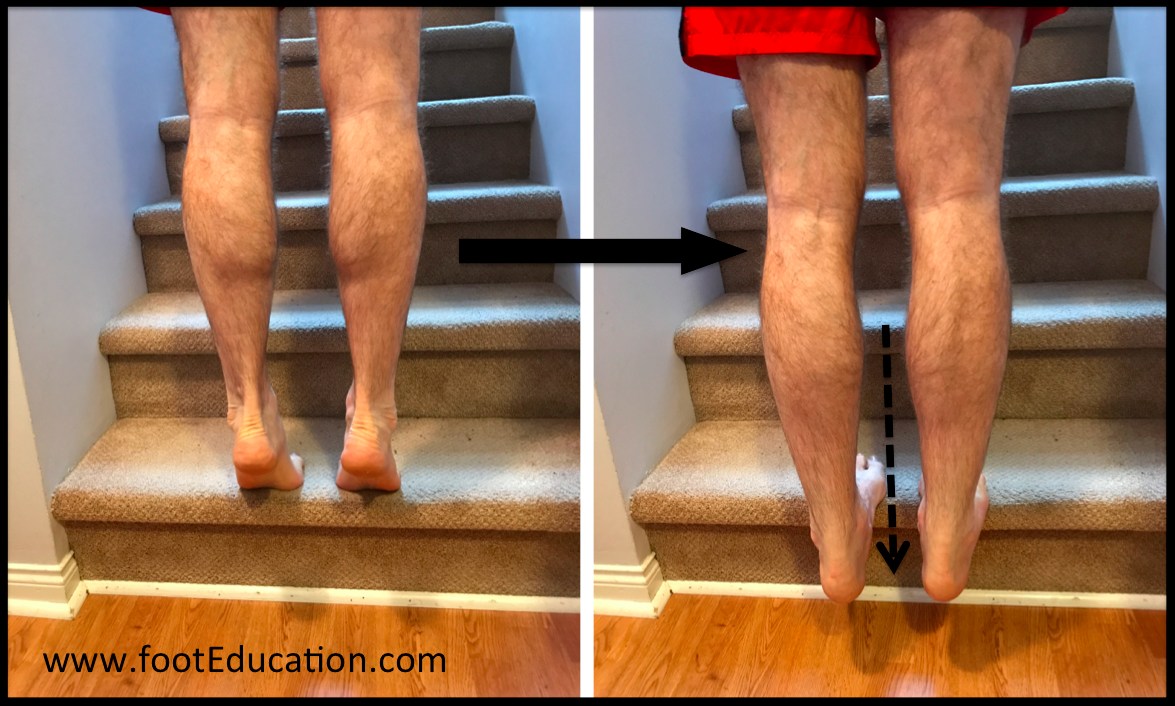
- Eccentric Achilles Tendon Exercises (ex. Heel Drops). Controlled exercises where the Achilles tendon is being lengthened while the calf muscle contracts have been shown to be very helpful in improving the symptoms associated with Achilles tendonitis. An example of this type of exercise is a “Heel drop”, where the patient stands on their toes while positioned on the edge of a ledge, such as a stair (Figure 5). Patients then slowly lower their heels down below the ledge, simultaneously stretching and strengthening the Achilles tendon. This can be done with both legs at the same time (bilaterally) or for a more concentrated effort, one leg at a time. It can also be done with the knees straight (putting force on the gastrocnemius) or with the knees bent (putting force on the soleus). Patients should gradually work up to performing 5 sets of 10 repetitions. These exercises should be performed 5-6 days per week during the active treatment phase, and then 3 times per week to minimize the chance of developing recurrent symptoms. It is CRITICAL that this exercise be approached cautiously, as these exercises have the potential to put excessive pressure on the Achilles. Patients should always warm up first (ex. get their blood flowing on an exercise bike for 5-10 minutes) before performing these exercises. (Figure 5)
- Platelet-Rich-Plasma (PRP) injections. It has been proposed that injecting platelet-rich plasma (PRP), taken from the patients’ own blood, may stimulate healing. However, there is a lack of evidence supporting that notion that PRP injections are more effective than traditional treatment options –or even when compared to placebo treatments. Corticosteroid injections are generally not recommended due to the increased risk of tendon weakening or even rupture.
Treatment of Achilles Tendonitis: Surgical Treatment
Surgery to treat Achilles tendonitis is usually not needed. It is only considered when appropriate non-operative treatment has fail. Patient compliance and postoperative management are important factors in preventing ankle stiffness or recurrence of the symptoms. Surgery usually requires removal of the damaged tissue (debridement) and possible repair of the tendon. In some cases of extensive damage, transfer of a local healthy tendon to augment the diseased Achilles tendon is helpful. Postoperative immobilization is required, followed by the gradual introduction of range of motion and strengthening exercises. It may require 6 months or more to achieve full recovery. Some known complications are recurrence, stiffness of the ankle, and deep vein thrombosis.
Printable Handout (Summary of Achilles Tendonitis)
Printable handout (complete webpage)
Edited on October 29th, 2024
Previously edited by Anthony Van Bergeyk, MD, Matthew Buchanan, MD, and Dr. Peter Stavrou, MD