5th Metatarsal Shaft “Dancer’s” Fracture
Summary
A twisting injury to the ankle and foot may cause a long oblique fracture of the 5th metatarsal shaft — the bone that attaches the little toe to the midfoot (Figure 1). During this injury, the 5th metatarsal is twisted by a strong force resulting in a spiral fracture. This 5th metatarsal shaft fracture is sometimes called a “Dancer’s fracture”. The injury causes localized pain, swelling, and difficulty walking. In many instances, this type of fracture can be treated non-operatively, with relative immobilization in a walking boot combined with limited weight-bearing. It typically takes about 6 weeks for adequate bone healing to occur, before patients can start to significantly increase their activity level. It often takes 4 or more months for a full recovery to occur.
**There is another fracture (5th metatarsal avulsion fracture) that may also be referred to as a dancer’s fracture. However, since this fracture of the fifth metatarsal was first described in ballet dancer’s, it has become known as a dancer’s fracture as well.

Clinical Presentation
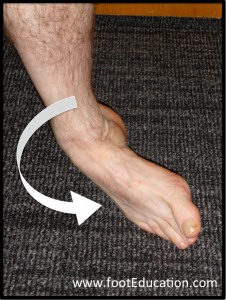
A patient who suffers a 5th metatarsal shaft fracture (See Figure 1) commonly gives a history of a twisting and loading injury to their ankle and foot (inversion and plantarflexion injury), similar to what occurs with an ankle sprain (Figure 2). An acute rolling of their ankle while pointing the toes down can also fracture the shaft of the 5th metatarsal (See Figure 1). This will produce immediate pain over the outside aspect of the foot near the toes. It can be associated with significant swelling. Weight bearing on the injured foot may be difficult due to pain and discomfort. Over time, the skin can turn black and blue. The injury is associated with quite specific local tenderness over the bone near the base of the fifth toe and on the outside of the foot (the 5th metatarsal).
Physical Examination
When pressing on the outside of the foot, there will be marked tenderness over the 5th metatarsal. There may be tenderness and swelling over a large area of the outside of the foot. However, the main tenderness will usually be just before the base of the fifth toe.
Imaging Studies
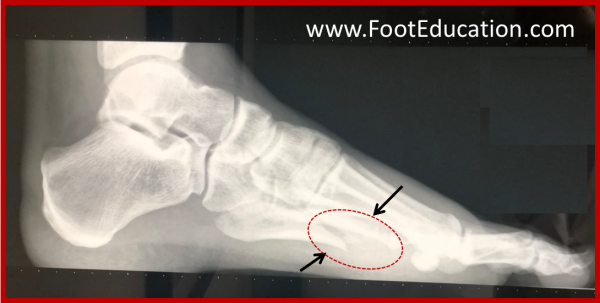
X-rays of the foot will reveal a long oblique fracture of the shaft of the 5th metatarsal. The size of the fractured fragment may vary considerably. There will be gapping at the fracture and there may be some shortening or rotation of the fracture (Figures 3A-3B). The usual fracture pattern is a spiral running from the outside aspect of the bone (distal lateral) near the toes to the inside aspect of the bone near the ankle (proximal medial).

Treatment
A 5th metatarsal shaft “Dancer’s” fracture is an injury that is usually treated non-operatively. The fracture has a very high rate of healing with non-operative treatment. Treatment involves relative rest and time to allow the fracture to heal. Typically, patients are placed in a walking boot. Although weight bearing is allowed, for the first few weeks, they will have to significantly limit their walking and may need crutches due to pain and discomfort. As the swelling settles and the fracture starts to heal, they can begin walking more extensively in the boot. Usually by 6 weeks, there is enough healing to allow them to transition to a stiff-soled shoe with lots of padding. This is a frustrating injury because it takes a long time for healing to occur. Patients are often still symptomatic 6 to 8 weeks or more after this injury. They can usually resume dance activities by 10-12 weeks and return to performance level by 19 weeks. It can be many months before the bone is completely healed and a full recovery has been achieved.
Surgery may be needed when there is complete displacement of the fracture fragments or failure to heal with non-operative treatment after several months. In these cases, the bone fragments are repositioned and stabilized with screws and/or a plate.
It is important not to overlook potential other associated injuries to ligaments of the ankle and foot.
Edited September 18th, 2023
Previously edited by David Oji, MD and David N. Garras, MD