Anterolateral Ankle Impingement
Summary
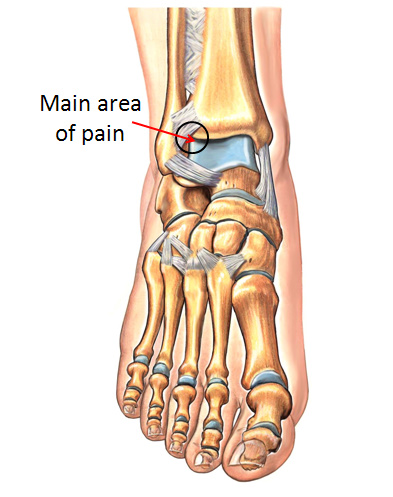
The hallmark of anterolateral impingement is pain located in the front outermost aspect of the ankle (Figure 1). This pain can often be made worse when a patient bends their ankle upwards. This condition is most commonly the result of soft tissue scar buildup in this location after a prior injury to the ankle (ankle sprain, high ankle sprain, ankle fracture). The redundant scar tissue effectively gets pinched or “sandwiched” between the bones of the ankle joint as the available space decreases during certain ankle movements (dorsiflexion). The pain is usually quite localized, and pressing on this area while moving the ankle joint will usually reproduce symptoms. Anterolateral ankle impingement is best diagnosed based on a good clinical exam. Non-operative treatment typically include avoiding aggravating activities, icing, and/or bracing the ankle. Patients that do not respond to such measures often become candidates for arthroscopic surgery, which is a procedure to clean out the scar tissue in this region of the ankle.
Clinical Presentation of Anterolateral Ankle Impingement
Pain at the front and outside aspect of the ankle joint (“anterolateral” region) is the main feature of anterolateral ankle impingement (Figure 1). This pain is often precipitated when the leg is bent forward over the ankle (dorsiflexed). There may be a history of a twisting ankle injury in the past. The location of the pain is quite discrete, and can be associated with a fullness or swelling which is very specific to this area. Pressing on the outside (lateral) aspect of the ankle joint line and bringing the foot upwards (dorsiflexing) will usually recreate the symptoms. In some patients there may be associated looseness in the ankle joint (ankle instability).
What is the Cause of Anterolateral Ankle Impingement?
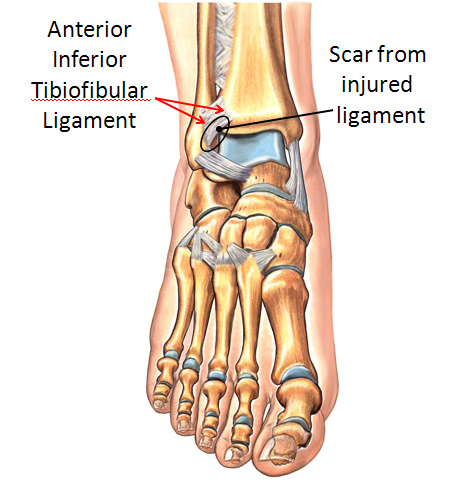
Symptoms from anterolateral ankle impingement occur when there is a build-up of scar tissue in the outer (lateral) aspect of the ankle joint. When the foot is brought upwards, the lower bone of the ankle joint (the talus) jams or “pinches” this scar tissue buildup between it and the upper bones of the ankle (the fibula and tibia). This impingement can be quite painful. When this occurs, it is classically the result of a prior ankle sprain. This injury tears one or more ligaments along the outer aspect of the ankle. The ligament most commonly associated with this problem is called the anterior inferior tibiofibular ligament (Figure 2). The anterior inferior tibiofibular ligament is one of the ligaments that holds the two bones of the lower leg together at the level of the ankle. Tearing of the lower bands of this ligament can produce a prominent mass of scar tissue leading to impingement. The anterior inferior tibiofibular ligament is the main ligament that is injured in a “high ankle sprain.” Therefore, anterolateral ankle impingement is one possible consequence of a high ankle sprain.
Imaging Studies
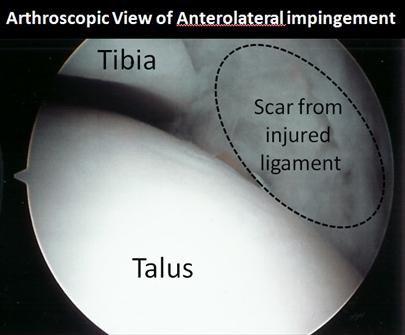
In general, anterolateral ankle impingement (or ALIS, as it is sometimes called) will not be identified on plain x-rays, and may also be missed on an MRI. When anterolateral ankle impingement is observed on an MRI, it is usually seen on the axial view (Figure 3). Typically, this diagnosis is made based on the patient’s history and the localized tenderness on physical examination. The diagnosis is sometimes confirmed by a diagnostic corticosteroid injection, which can also often be therapeutic. If the symptoms persist, the diagnosis can be confirmed during arthroscopic surgery where the actual jamming (impingement) can be observed (and treated).

Treatment of Anterolateral Ankle Impingement
Non-Operative Treatment
True anterolateral ankle impingement is the result of a physical impediment inside the ankle joint that affects the functioning of the joint. Fortunately, non-operative management is often quite effective in treating this problem. Various treatment options which may be helpful include:
- Use of a shoe with a slight heel: By using a slightly increased heel, there is less chance that the foot will be forced upward enough to cause the jamming at the joint.
- Activity Modification: Sometimes the most effective treatment is to simply avoid the activities that precipitate symptoms. It is not uncommon for patients with anterolateral ankle impingement to have only certain specific activities (i.e. crouching down) that aggravate symptoms, and if these can be avoided then it may be possible to effectively manage this condition non-operatively.
- Using an Ankle Brace or Taping the Ankles: Limiting ankle motion, either by using an ankle brace (ankle lacer) or by taping the ankle, will tend to limit ankle motion and may prevent the ankle joint from jamming.
- Anti-inflammatory medications (NSAIDs) may decrease the inflammation within the joint and allow the process to subside.
- Injecting the Ankle Joint: An injection of corticosteroids into the ankle joint can sometimes help symptoms significantly. If the repetitive jamming has caused the ankle joint lining (synovium) to be inflamed, then a corticosteroid injection may allow this inflamed tissue to settle with resulting improvement in symptoms.
Operative Treatment
Surgery for true anterolateral ankle impingement ankle joint can be very effective if non-operative treatemtn has not been successful. When surgery is required to improve this problem, arthroscopy has traditionally been the treatment of choice for the surgeon. Arthroscopic surgery utilizes a tube-like camera and fine custom designed instruments to enter the ankle joint through small keyholes (Figure 4). The scarring that causes anterolateral ankle impingement can also be removed by larger incisions using a more formal open approach to the ankle. Such additional surgery is generally only used if other surgeries on the ankle are being performed that cannot be done arthroscopically.
Arthroscopic Surgery for Anterolateral Ankle Impingement
Placing an arthroscope inside the ankle joint allows the surgeon to inspect the entire ankle joint, which is a tremendous advantage in the event that there are other problems elsewhere in the ankle. It also permits direct visualization of the impinging soft-tissue scar when the foot is flexed up (dorsiflexed). Sometimes, the repetitive jamming will have caused some of the cartilage on the outside of the talus (lower bone of the ankle) to be worn away. Sometimes, other ankle problems such as a talar osteochondral lesion or ankle instability will also be found present and will need to be addressed surgically at the same time.
Recovery
Surgery for ALIS generally works quite well and can provide a predictable return to function with good pain relief. If surgery involves only cleaning up the scar tissue along the outer aspect of the ankle, then the recovery is often fairly quick. There is usually a 6-8 week period of increased ankle pain and swelling, during which time the patient may have a limping gait. Full recovery can, however, take 3-6 months or longer.
When there are other things going on inside or around the ankle joint (ex. Talar Osteochondral lesion, ankle arthritis, peroneal tendonitis, ankle instability, etc.) additional surgery may be required. In this case the recovery from surgery may take much longer. The implications and severity of these additional findings can obviously affect long-term outcome.
Potential Surgical Complications
General Complications
This type of arthroscopic surgery typically has a very low complication rate, and the procedure is typically performed as an outpatient (not overnight) procedure. However, as with all orthopedic surgery, risks include:
- Infection
- Wound healing problems
- Blood Clots or Pulmonary Embolism
- Nerve irritation or injury (An indirect injury to the superficial peroneal nerve, leading to neuritis or neuroma)
- Traction injury (tendonitis or skin irritation/abrasion from the distraction used to get a good look inside the joint space)
- Persistent symptoms.
Edited on February 20th, 2024
Originally edited by Paul Juliano, MD
sp/2.20.24