Osteochondral Lesion of the Talus (OLT)
(aka Talar OCDs or Talar OCLs)
Edited by Matthew Buchanan, MD
Summary
Watch Video: Osteochondral Lesion of the Talus (OLT or OCD)
An osteochondral lesion of the talus (OLT) is an area of abnormal, damaged cartilage and bone on the top of the talus bone (the lower bone of the ankle joint). This condition is also known as either osteochondritis dissecans (OCD) of the talus or as a talar osteochondral lesion (OCL). It is often associated with a traumatic injury, such as a severe ankle sprain. However, it can also occur from chronic overload due to malalignment or instability of the ankle joint.
OCLs most commonly occur in two areas of the talus (Figure 1A and 1B):
- The inside and top part of the lower bone of the ankle (the medial talar dome) or
- The outside and top part of the lower bone of the ankle (the antero-lateral talar dome).
Figure 1: MRI of Medial (Inside) Talar OLT
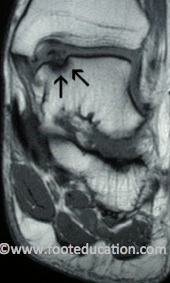
Figure 1B: MRI of Lateral (Outside) Talar OCL

Clinical Presentation
Many patients with talar OLTs are asymptomatic (no pain or swelling). OLTs can be an incidental finding on an MRI ordered to assess another problem. However, if the lesion is large enough, or the overlying cartilage is displaced, talar OLTs can be quite symptomatic. These symptoms could include localized ankle pain, as well as discomfort on either the inside (medial talar OLT) or outside (anterolateral talar OLT) of the ankle. The pain is often worse with activities, particularly running, walking and jumping. They may also complain of mechanical symptoms, such as clicking and popping sounds caused by a loose fragment of cartilage and/or bone associated with the OLT.
OLTs on the top outside part of the talus (Antero-lateral lesions) usually have a history of a traumatic injury with a twisting component, such as an ankle sprain. Whereas, the OLTs on the inside part of the top of the talus (medial talar osteochondral lesions) are more commonly associated with chronic overload of the medial aspect of the ankle, such as would occur in a patient with a higher arched foot (subtle cavus foot). Physical exam usually reveals some swelling and localized pain along the front of the ankle (ankle joint line).
Imaging Studies
Plain x-rays can be used to help diagnose an osteochondral lesion. Areas of decreased density (i.e., darker areas) seen on the plain x-rays (Figure 2) can be indicative of this condition, although it is not uncommon for the plain x-rays to be read as normal. The gold standard for diagnosis of talar OLTs is an MRI of the ankle (Figure 3A and 3B). An MRI of the OLT may show that the cartilage and bone damage is displaced (out of position) or non-displaced (perfectly in position).
Figure 2: Medial Talar OLT on plain X-Rays

Figure 3A: MRI Lateral (side) view of Talar OLT

Figure 3B: MRI Anteroposterior (view from front) of Talar OLT

Treatment
Non-Operative Treatment
Non-operative treatment can be successful for non-displaced talar OLTs, especially if the condition is recognized and treated early, and the lesion is relatively small. Younger patients, particularly growing children or adolescents, have a much better chance of healing an OLT compared to adults. There are several non-operative management options for the treatment of osteochondral lesions, including:
- Cast immobilization: If the OLT occurs following an acute injury, initial immobilization in a cast for 4-6 weeks can help reduce stress on the OLT and allow healing. This treatment approach can be initially attempted in non-displaced OLTs.
- Physical therapy: working on strengthening the muscles around the ankle, range of motion of the ankle, and balancing (proprioception)
- Protective braces (ex. Ankle Lacer) to decrease stress can also be utilized.
In younger patients, this condition has the potential to heal, making it possible to treat acute non-displaced talar OLTs with immobilization in a cast or CAM walker.
Operative Treatment
Surgical treatment is indicated for displaced talar OLTs or lesions that have not improved with appropriate non-operative management. Surgical treatment of talar OLTs includes:
- Arthroscopic debridement (cleaning out) and microfracture of the talar OLT. This is the standard operative treatment and leads to good or excellent results in 75-80% of patients with typical talar OCLs (less than 15mm²)
- Osteochondral Autologous Autograft Transfer (OATs Procedure) An OATs-type procedure is reserved for patients who have been treated with arthroscopic cleaning out (debridement) and microfracture and are still not doing well, or patients that have a very large (>20mm²) talar OLT. This procedure may also be called a mosaicplasty. The theoretical advantage of this procedure is that it replaces the damaged cartilage with cartilage and bone harvested from the patient (autograft). The graft is usually harvested from the patient’s knee on the same leg, from an area of that joint that does not bear any load. Patients can develop knee problems after this procedure. The main disadvantage of this procedure is the prolonged recovery time and increased complication rate, compared to arthroscopic debridement.
- Osteochondral Allograft Transfer (i.e., Cadaver): A bone and cartilage plug may also be obtained from a cadaver and transplanted into the OLT. This prevents the need from harvesting bone and cartilage from another part of the body (ex. knee). Osteochondral allografts (Cadaver grafts) have been used to treat large talar lesions with some success. However, the larger the graft, the more likely it seems that it will collapse as a new blood supply is established into the graft after transplantation.
- Autologous chondrocyte transplantation (ACI): There has been an attempt to harvest a patient’s own healthy cartilage, grow the cells in a lab, and then reimplant these cells back into the area where the cartilage has been lost. Unfortunately, this approach in the ankle has not yet met with the type of clinical success that had been hoped for, and is not currently broadly available. Laboratory and clinical work continue in this area.
Other Procedures
Any other significant pathology that exists may also need to be addressed at the time of surgery. This may include:
- Surgery to address ankle instability, such as a Brostrom Lateral ligament repair or a lateral ligament tendon reconstruction.
- Calcaneal osteotomy to address significant hindfoot alignment abnormalities (usually hindfoot varus treated with a lateralizing calcaneal osteotomy)
Edited July 31, 2017
Previously edited by Kenneth Hunt, MD
mf/ 9.23.19