Neuritis and Neuromas of the Foot and Ankle
Edited by Eric Malicky MD
Clinical Presentation
Injury or irritation to nerves in the foot and ankle often creates pain and/or numbness. They occur as a result of an injury to a specific nerve. Nerve damage can result from the original injury, casting/wrap, or surgery. Symptoms often include a burning pain along the course of the nerve, but may also be associated with numbness over the sensory area that the nerve supplies.
There are five main nerves that go past the ankle (Figure 1) and these nerves and their various branches can be injured creating nerve-type (neuritic or “electric/shock-like”) symptoms. Many neuromas occur following foot or ankle surgery. In some instances, nerves are inadvertently cut or injured although more commonly bleeding from an operation or injury can cause scarring around the nerve. Symptoms of varying severity can occur.
Figure 1: 5 Common Nerves of the Foot and Ankle
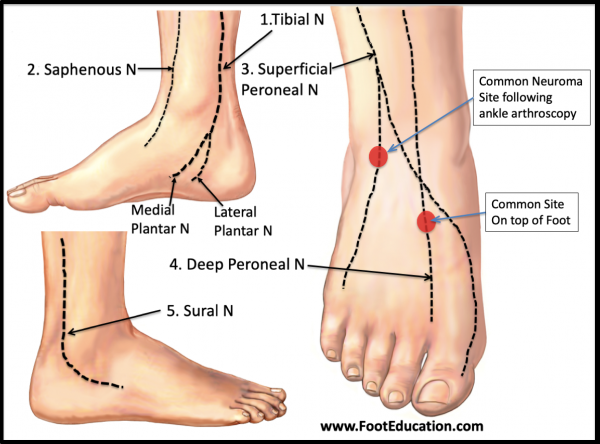
A common sites of neuroma formation following ankle arthroscopy surgery is the front outside part of the ankle (Figure 1) where the incision for the outer portal is created. Another common site of neuroma formation is the top of the foot (Figure 1) due to direct pressure from a bone spur (tarsal bossing) or from external pressure from tight fitting shoe laces.
In patients with a neuroma, the most common finding on physical exam is localized discomfort –often burning in nature. If the injured area is lightly tapped a shooting sensation along the course of the nerve is often created. This is called a positive Tinel’s sign. In addition, it is common to find an area of numbness or abnormal sensation over the distribution that the nerve supplies. Evidence of a previous incision from surgery or scar from an injury is also commonly seen. In some patients where excessive repetitive excitement of the injured nerve has started to affect other nerves in the foot the foot itself may have some general redness and the skin may appear somewhat shiny. When rubbed the reddish skin may blanche white (dermatographia). Extreme examples of this may represent signs of a complex regional pain syndrome (CRPS).
Imaging Studies and Investigations
X-rays: Often normal or demonstrate signs of a previous operation. The injured nerve is not going to be seen on an x-ray.
MRI: may show increased scarring, but many nerves are too small to be seen on MRI.
NCV/EMG: A nerve conduction study (NCV/EMG – nerve conduction velocity/electromyography) can show abnormalities of larger nerves or reveal other underlying causes of nerve injury (ex. Lumbar spine compression on nerve roots or polyneuropathy). Unfortunately, many of the small nerve branches of the ankle/foot are isolated sensory structures and won’t be detected on the NCV/EMG.
Diagnostic Injection: using local anesthetic along the nerve branch above the area of pain can often clarify the source of pain.
Types of Nerve Injuries
There is a spectrum of nerve injuries which range from mild irritation to the outside of the nerve to a complete disruption of the nerve. In mild cases of nerve injury, scar tissue surrounds the nerve and increases the sensitivity from this area. In this case, the nerve structure is normal but the surrounding irritation effects the signal (similar to mud surrounding a hose which effects the water flow). The second type of nerve injury involves a direct injury to the small nerve fibers while maintaining the outside sheath. This results in a partial nerve injury with more severe pain. The third type of nerve injury results in a complete disruption of the nerve structure. The cut/torn nerve will no longer transmit normal sensation or stimulate its muscles. This condition can be difficult to diagnose but most characteristic of severe point pain (at the site of nerve injury) causing a “electric/shock-like” pain.
Complex regional pain syndrome is rare, but can be initiated from any type of injury to a nerve. The result is a global hypersensitivity of the involved ankle/foot even with mild stimuli (ex. bedsheets hurt the feet sleeping).
Treatment of Neuromas in the Foot
Early diagnosis and treatment are critical when dealing with foot/ankle nerve injuries. Treatments include:
Physical Therapy: desensitize the neuroma
The therapist and patient can massage the area around the nerve to gently break up scar. Although this may initially be uncomfortable, the results can slowly settle down irritated nerves. Sound judgment is needed to not “overdo” the nerve stimulation. Start with a light warm wash rag and gently rub the area.
Local Anesthetic Patches
A trial of a lidocaine patch to the sensitive area of the foot/ankle can help minimize nerve pain. Consider applying the patch to the skin daily for 1-2 wks to determine efficacy.
Nerve Quieting Medications
Some medications can slow the pain message from the nerve to the brain. These drugs need to be monitored and although beneficial, can have annoying side effects.
Neuroma Surgery
There are several surgeries available to help improve neuroma symptoms including cutting the painful nerve segment and burying its stalk into muscle or bone.
Lumbar Sympathetic Blocks
In the unusual case of reflex sympathetic dystrophy an injection in the lower back can settle down the intense pain. Often a pain physician specialist will administer this treatment.
Avoid Local Irritation
Often an irritated nerve can be worsened from external pressure. If you notice this pattern, try and loosen the shoe/ankle brace around the painful neuroma (ex. Loosen the shoe laces for top of foot nerve pain).
Edited February 11th, 2019