Morton’s Neuroma
Watch Video: Morton’s Neuroma
Clinical Presentation
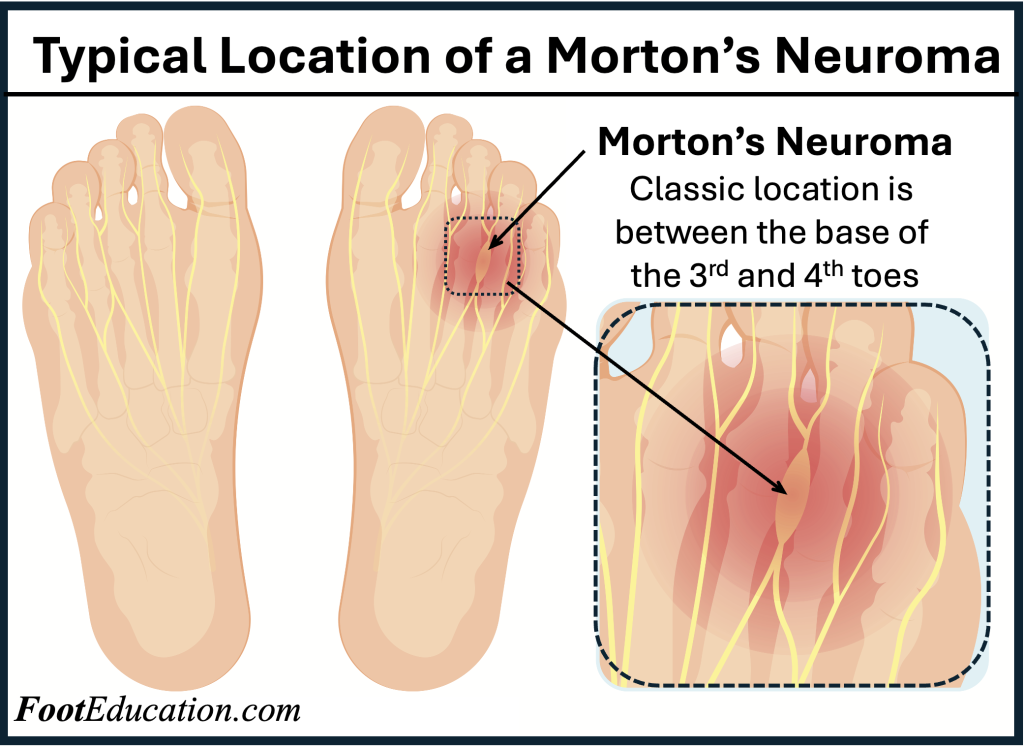
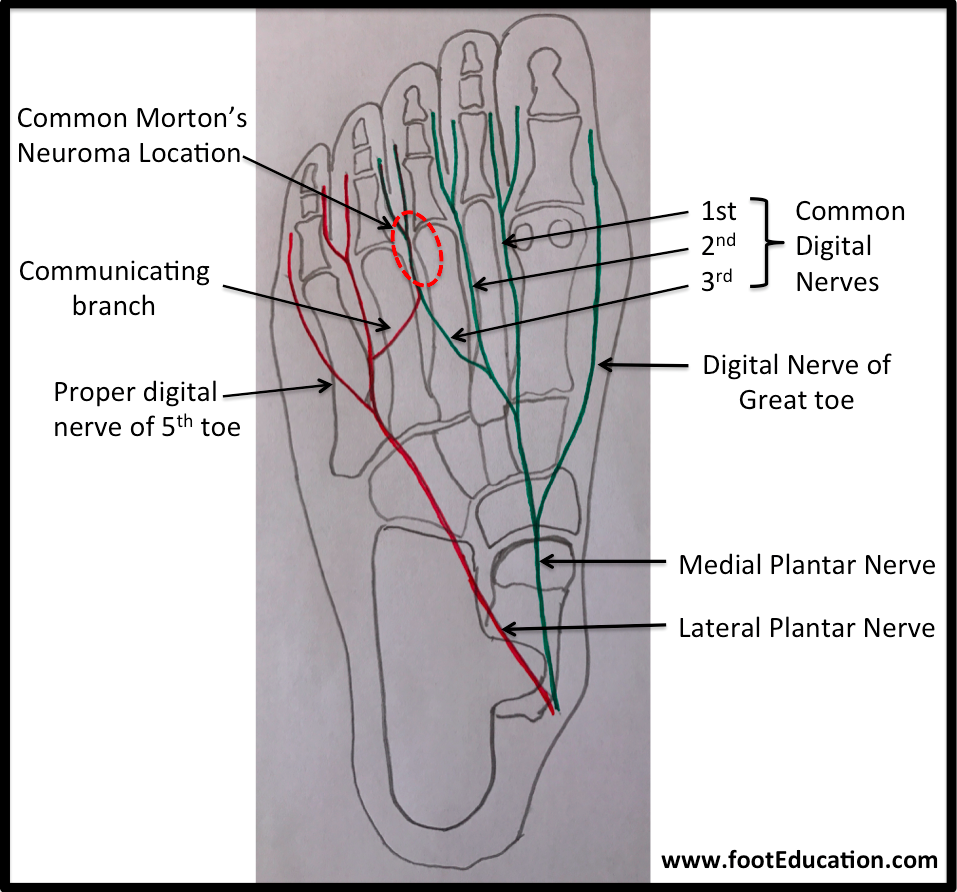
Patients with Morton’s neuroma present with pain in the forefoot, particularly in the “ball” of the foot (figure 1). The pain is classically located near the base of the 3rd and 4th toes. However, not all pain in the forefoot is a Morton’s neuroma. In fact, most chronic pain in the forefoot is NOT the result of a Morton’s neuroma, but rather is from inflammation (synovitis) of the “toe/foot” joints in a condition known as metatarsalgia. The symptoms of Morton’s neuroma are due to irritation of one of the small nerves, just before it travels into the toes (Figure 2). The symptoms of a Morton’s neuroma include pain, numbness (usually between the 3rd and 4th toes) and sometimes a burning sensation.
In many cases, a neuroma may develop as a result of excessive loading on the front of the foot. Such a loading for example can occur in those who regularly wear high heels with a narrow toe box. Sometimes, a patient’s anatomic alignment in the forefoot contributes to the overload. There may be some cases where the neuroma develops spontaneously, for no obvious reason. However, once the nerve is irritated, pressure from walking, and from the adjacent bony prominences (metatarsal heads) may contribute to persistent pain. Patients will feel pain that worsens with walking, particularly when walking in shoes which are narrow, with thin soles, or high heels. Patients will often feel more comfortable out of shoes.
Physical Examination in Morton’s Neuroma
Patients with classic Morton’s neuroma symptoms will have pain with pressure at the base of the involved toes –usually the 3rd and 4th toes. In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe, usually in between the 3rd and 4th toe, as this corresponds with the distribution of the involved nerve. Ultrasound or MRIs are the best way of showing a neuroma. Plain x-rays of the foot may demonstrate that one or more of the metatarsals are long
Treatment of Morton’s Neuroma
Most non-operative treatment of Morton’s neuroma is usually successful, although it can take a while to figure out what combination of non-operative treatment works best for each individual patient. Non-operative treatment is similar to the treatment of metatarsalgia in general and may include:
- The use of comfort shoe wear.
- The use of a metatarsal pad to decrease the load through the involved area of the plantar forefoot.
- A period of activity modification to decrease or eliminate activities, which may be exacerbating the patient’s symptoms. For example, avoiding long periods of standing or other activities that result in significant repetitive loading to the forefoot can be very helpful. Wearing high heels should be avoided.
- Local corticosteroid injections can help decrease pain and inflammation associated with the nerve. However, this does not necessarily address the underlying loading forces that may be causing the injury to the nerve in the first place.
Surgical Treatment of Morton’s Neuroma
Operative treatment of Morton’s neuroma should be considered only after failure of non-operative management and only if it can be ascertained that the symptoms are not primarily due to any other pathology such as inflammation of the nearby joints (metatarsalgia). Standard operative treatment involves identifying the nerve and cutting (resecting) it above the point where it is irritated/injured. This is usually done through an incision on the top (dorsal) aspect of the foot, although an incision on the sole (plantar) aspect of the foot can be used.
Some physicians will attempt to treat Morton’s neuroma by releasing the intermetatarsal ligament, and freeing the nerve from the pressure under the ligament or any local scar tissue. This may also be beneficial. The ultimate success of a Morton’s neuroma treated surgically can be variable. In cases where the underlying problem is only an irritated nerve (a true Morton’s neuroma), then surgery is usually successful (although it may take a few months for the foot to fully heal). But in many cases, forefoot pain is more complex. There may be an irritated nerve or two causing pain, but the real problem is often excessive loading of the lesser metatarsals. The generic term for this condition is metatarsalgia. When considering surgery, identifying and addressing these problems may lead to a better end result.
Potential Surgical Complications
Potential operative complications include:
- Delayed healing. It is not unusual for mild residual swelling at the surgical site to cause persistent discomfort for 2-3 months.
- Infection.
- Wound healing problems. Wound healing problems can be particularly problematic if the incision is on the plantar surface of the foot, as scars in this area can be quite troublesome.
- Stump Neuroma. Where the nerve regrows where it has been cut causing recurrence of symptoms.
- Deep Vein Thrombosis (DVT).
- Pulmonary embolism (PE).
- Continued pain. This is not uncommon as the nerve maybe only a part of the pain generating complex.
- Reflex sympathetic dystrophy or complex regional pain syndrome – (CRPS). In some instances, an aggravation of the nerve, such as what may occur at the time of the surgery, can lead to the development of a complex regional pain syndrome, which can be quite troublesome. Fortunately, this complication is relatively uncommon.
Edited by Stephen Pinney MD, March 5th, 2025
Previously edited by Dave Townshend, MD, Vinod Panchbhavi, MD, and Justin Greisberg MD