Scar Massage using Soft-Tissue Mobilization or Myofascial Release
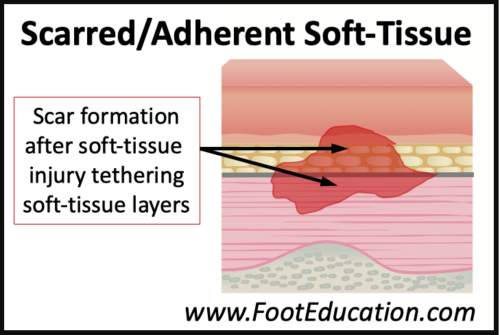
Scars form in the soft tissue after local injury or bruising. Imagine scraping your knee and seeing blood ooze from the wound. The blood will soon congeal, a scab will form, and over time the wound will heal with local scarring. A similar process occurs for injuries below the skin. A strained muscle, ligament tear, broken bone, or soft tissue contusion will all produce bleeding into the local soft tissues. This bleeding will often show itself as bruising. The blood will congeal and over time it will be resorbed by the body. As the soft-tissue injury matures the color will change with time which is why bruises go from dark bluish-purple, to yellow-green, and then light brown. However, these soft tissue injuries often leave a scar causing various tissues to stick together. As a result, these layers of soft-tissue do not move past each other as smoothly as they did prior to the injury. Scar massage using soft tissue mobilization techniques such as myofascial release can be very helpful to free up this type of soft tissue scarring.
Soft-tissue Mobilization: General Strategy or as a Specific Intervention
The treatment strategy of soft tissue mobilization encompasses a variety of different techniques including scar massage and myofascial release. Soft tissue mobilization can be used as a general treatment strategy or as a specific intervention. Used as a general strategy soft-tissue mobilization (ex. massage) involves mobilizing all of the muscles and soft tissues in an extremity to maintain their pliability and length as well as ensuring that various tissue layers continue to move smoothly past each other. As a specific treatment strategy, soft-tissue mobilization focuses on releasing areas of soft tissue scarring resulting from a local injury. It is this more specific focal breaking up of local soft-tissue scar and adhesion formation that will be discussed in this article.
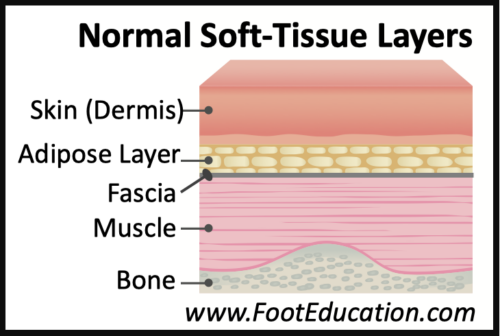
Soft-Tissue Layers
To understand how soft tissue mobilization works to treat local scar formation. It is important to understand soft tissue anatomy. From the skin down to the bone there are a series of soft tissue layers (Figure 1). These include the skin or dermis, and deep to this is the fatty adipose tissue layer. Deep to the adipose tissue is often a facial layer. The fascia is a strong fibrous tissue that holds the muscles in place. The muscles and their tendons are deep to the fascial layer and they attached to the bone which represents the deepest structure. The skin, adipose layer, fascial layer, and muscles constitute the soft tissues. Running throughout these soft-tissues are other structures including blood vessels, nerves, and tendons. Normally, the various soft tissue layers glide smoothly and easily over each other. However, with acute or chronic injuries adhesions and scarring can build up in the soft-tissues (Figure 2) which can limit the normal gliding of the soft-tissue layers causing local discomfort, impairment of muscle function, or irritation of local tendons (tendonitis) or nerves (neuritis).
Soft-Tissue Mobilization Techniques
When an injury causes local soft-tissue scarring or adhesions to form soft-tissue mobilization is often the most effective treatment. The patient may perform this scar mobilization or myofascial release. However, more aggressive mobilization may be more effectively be performed by a physical therapist, who may use specialized techniques or skills to help break up stubborn scar tissue. The general goal is to break up the adherent scar tissue, so that the layers of soft tissue can easily glide past one another. There are a variety of soft tissue mobilization techniques that can be used. The use of the hands to directly manipulate the scarred area is common. This is one of the hallmarks of myofascial release. The goal is to break down the scar tissue that has formed between the various soft tissue layers. There is always a balance between being overly aggressive which can be painful and lead to additional local soft tissue bleeding and more scar formation versus manual therapy that is to passive and will not appreciably alter the scar tissue that has formed. Often treatment needs to be carried out for a number of sessions over a number of weeks to successfully mobilize the scarred area. Other soft tissue mobilization techniques use instruments such as smooth stainless steel curved bars (Figure 3) to help manipulate and mobilize the scarred, soft tissue. Cupping is another technique that may be employed. Cupping uses a suction cup to help separate the soft tissue layers when adhesions have formed. A patient may use foam rollers or tennis balls on their own to provide localized pressure on their soft tissues. This direct pressure on the soft-tissues can help break up areas of adhesions as well as allow the local to relax and stretch.

For patients with symptoms related to soft tissue scarring following an injury a course of soft tissue mobilization, overseen by a trained physical therapist can be very effective. Although it can take some time to see the results of this treatment. Continued home use of a foam roller or tennis ball to keep all of the muscles loose and minimize the risk of recurrent scar formation can be a very effective on-going treatment strategy.
March 4th 2024