Insertional Achilles Tendonitis
Also: Retrocalcaneal Bursitis, Haglund’s Deformity, Posterior Heel Pain
Summary
The primary symptom described by patients with the terrible triad of posterior heel pain is pain in the back part of their heel (Figure 1). The terrible triad includes:
- Insertional Achilles tendonitis
- Retrocalcaneal bursitis
- A Haglund’s deformity
Patients may also have swelling that is quite tender to the touch. Standing, walking, and constrictive shoes typically aggravate symptoms. Many patients with this problem are middle-aged and some may be slightly overweight. Another group of patients who suffer from this condition are some active runners.
Summary Handout: Insertional Achilles Tendonitis

Printable handout: Insertional Achilles Tendonitis webpage
Background: The Terrible Triad of Insertional Achilles Tendonitis
1. Insertional Achilles Tendonitis
The Achilles tendon connects the calf muscle to the heel bone. As the strongest and largest tendon in the body, the Achilles tendon is regularly subjected to forces that are 2-4 times greater than a person’s body weight. The forces are even stronger during athletic participation, which means the Achilles bears an immense amount of stress on a regular basis. Over time, these repetitive loads can lead to degenerative wear and tear, specifically where the tendon inserts into the heel bone (calcaneus). This degeneration incites an inflammatory response and produces pain at the back of the heel. Eventually, the inflamed Achilles tendon may become calcified, forming bone-like fragments in the tendon (Figure 2 White Arrow).
2. Haglund’s Deformity
Haglund’s deformity is the bony prominence associated with the upper part of the heel bone (calcaneus). This prominent bone tends to form gradually over many years, and can eventually cause irritation by disrupting nearby structures, (Figure 2).
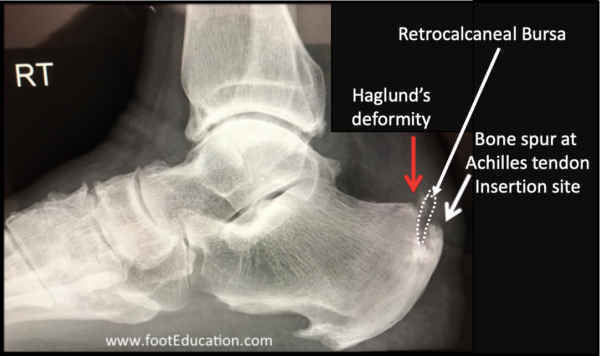
3. Retrocalcaneal Bursitis
Wherever tissues rub against one another, a bursa forms to allow for smooth gliding of tissues. A bursa is a sac filled with lubricating fluid, which occurs normally throughout the body. Although it is normally only a few cell layers thick, when irritated, a bursa can become markedly thickened and painful. This is often referred to as bursitis.
The retrocalcaneal bursa is positioned to allow the Achilles tendon to glide over the back part (posterior aspect) of the heel bone. When this bone becomes enlarged, inflammation of the retrocalcaneal bursa occurs. This inflammation results in exquisite tenderness along the posterior aspect of the heel.
Clinical Presentation: Insertional Achilles Tendonitis
Patients with posterior heel pain due to the terrible triad report tenderness over the back of the heel where the Achilles tendon inserts into the heel bone. The symptoms often come on gradually, although a sudden increase in activity level may start the symptoms. Patients experience swelling, and they may note a bump that is most irritated with tight fitting shoes. Running may aggravate the symptoms.
Physical Examination
There is tenderness and swelling on palpation of the heel when compared to the other side. Redness is occasionally present. Patients may walk with a limp or have may have difficulty taking a full stride. In long-standing cases, the tendon lengthens and a single leg heel rise becomes difficult.
Treatment of Posterior Heel Pain due to Insertional Achilles Tendonitis
Non-Operative Treatment
Initial treatment for posterior heel pain starts with non-operative treatment. Traditional non-operative treatment includes the following:
- Heel Lift or the Use of a Shoe with a Moderate Heel: Walking barefoot, or in a flat-soled shoe, increases the tension on the insertion of the Achilles tendon. Using a heel lift or a shoe with a moderate heel can help both reduce the stress on the tendon, and decrease the irritation caused by this condition.

- Calf Stretching: Regular calf stretching can help improve the compliance and length of the Achilles tendon. This makes it more resilient to wear and tear due to the repetitive loading associated with standing and walking.
- Nonsteroidal anti-inflammatories [NSAIDs] may help manage symptoms, but these medications do not address the actual underlying pathology. They work by limiting the body’s inflammatory response, and decrease the heel pain. If a patient has a history of stomach problems, such as an ulcer or heartburn, NSAIDs should be avoided or precautions taken. Recent data shows an elevated of risk of cardiovascular disease with prolonged use of these medications.
- Weight Loss: Many patients with posterior heel pain are overweight. A concerted effort to lose substantial weight may be one of the most effective ways to manage this condition. The Achilles tendon is often subjected to forces equivalent to many times a person’s body weight during regular, daily activities (i.e. walking and standing). Therefore, losing weight (even as little as 5-10 pounds) can be very helpful.
- Cast or Walker boot: Wearing a removable fracture walker boot for 4-8 weeks may permit healing of the degenerative tendon tearing. This is often successful initially, but if the cause of the microscopic tendon tearing is not addressed, the symptoms may recur.
Operative Treatment
Due to the lengthy recovery associated with surgery, along with the relatively unpredictable postoperative outcome, non-operative management should be exhausted before surgery is contemplated. However, in high-level athletes that have developed Haglund’s deformity from running, surgery may be indicated. Surgery usually involves:
- Removing the prominent excess bone associated with the Haglund’s deformity.
- Removing the thickened inflamed retrocalcaneal bursa.
- “Cleaning up” (debriding) the Achilles tendon. In some patients where there is excessive degeneration of the tendon, it is necessary to partially or completely remove the tendon and then reattach it. In these instances, it may be necessary to augment or even replace the completely degenerative Achilles tendon with another tendon, such as the big toe tendon (flexor hallucis longus).
Recovery from surgery is prolonged. Initially, the leg is immobilized to allow the wound to heal. Then gentle range of motion exercises can be started. Patients are protected from full weight-bearing for the first six weeks while the tendon heals to the bone. Gradually, with physical therapy, full weight bearing and return to activity can be expected. Improvement in strength continues for several months and may take over one year. The recovery is quicker in younger, athletic patients.
Potential Complications
Specific Complications
Complications that are specific to this surgery to treat insertional Achilles tendonitis include:
- Potential for partial or complete rupture of the Achilles tendon where it attaches (inserts) into the heel bone (calcaneus).
- Infection in the area of the Achilles tendon, although relatively uncommon, is a very serious problem due to the limited skin and soft-tissue coverage in this area.
General Complications
- Wound infection.
- Wound breakdown.
- Injury to the sural nerve.
- Deep vein thrombosis [DVT].
- Gait asymmetry leading to low back pain or other symptoms.
Printable handout
Edited October 29th, 2024
(Previously edited by Samuel G. Dellenbaugh, MD, Lance Silverman MD, and Tim Charlton MD)