Ankle Arthroplasty
(Ankle Replacement)
Indication
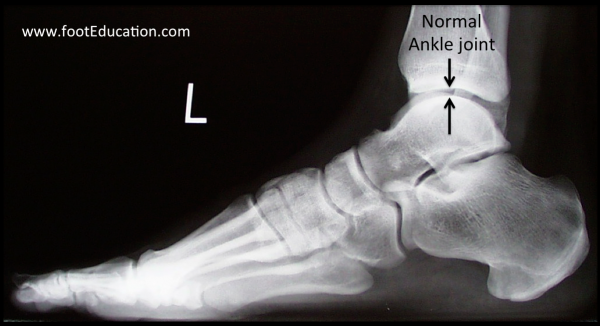
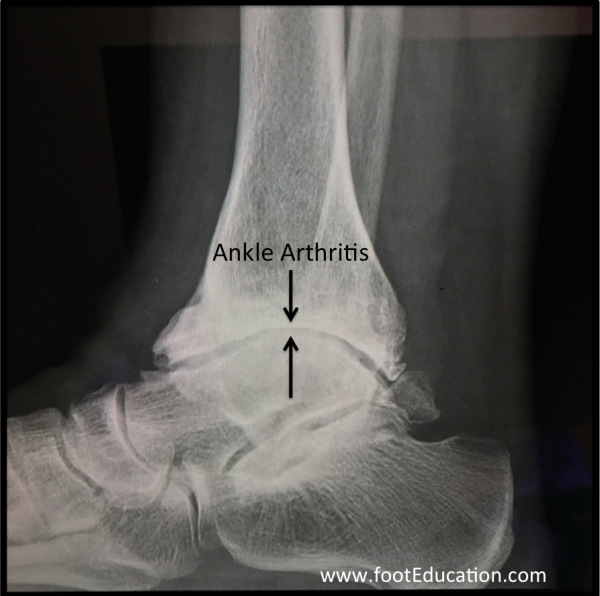
Ankle replacement surgery (also called ankle arthroplasty) is performed as a treatment for end-stage ankle arthritis (See Figure 1). Ideal surgical candidates for an ankle arthroplasty are often older, lower demand individuals. This is because the lifespan of an ankle replacement does not appear to be as long as for patients undergoing a knee replacement (~90% last 15 years) or a hip replacement (~90% last 18 years). However, newer ankle replacement designs appear to be lasting longer, so patients in their 50’s and even some patients in their 40’s now may be considered viable candidates for this procedure. Patients that have arthritis (or fusions) involving the joints below the ankle (ex. the subtalar Joint, talonavicular joint, and/or calcaneocuboid joints), may particularly benefit from an ankle replacement, as this procedure will help to preserve some hindfoot motion when compared with an ankle fusion.
Relatively young, active patients typically do not do well with ankle replacements in the long run. The higher forces going through the ankle joint (compared to the knee and hip joints), combined with the tendency for the ankle joint to be loaded unevenly predisposes ankle replacements to fail earlier than knee replacements and hip replacements. Furthermore, the limited bone stock around the ankle joint can make revision surgery notably more complicated. For these reasons younger patients with debilitating ankle arthritis are usually best served with a well performed ankle fusion. Newer ankle replacement designs and improved surgical techniques have improved the overall results following total ankle replacement surgery, although there is still room for improvement. Additionally, when considering whether a patient is a candidate for an ankle replacement the surgeon will assess not only the extend of ankle arthritis, but also any deformities in the foot. It is imperative that the foot and lower extremity be well aligned in order to achieve a good long-term outcome following an ankle replacement. The potential need to also surgically correct associated foot and lower extremity deformities can make ankle replacement surgery a greater challenge than hip and knee replacement.
Procedure
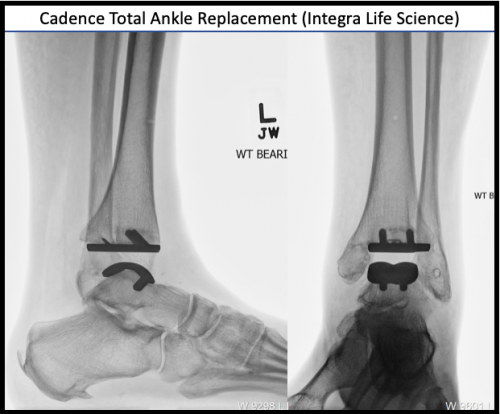
The surgical technique involved in performing an ankle replacement depends on the type of prosthesis that is used. In all ankle replacements, the arthritic surface of the upper part of the ankle joint (distal tibia) is removed, as is the arthritic surface of the lower bone of the ankle joint (the talus). Typically only the tibial surface and some of the talar dome are removed (Figures 2 and 3). The resected areas of bone are then replaced with the prosthesis. The prosthesis typically has a metal surface on the tibia, and talar sides with a polyethylene surface attached to the tibial component. The polyethylene surface does not show up on x-rays. It therefore creates the clear space between the metal prostheses that is seen on post-operative x-rays (Figure 2 and 3).
Contraindications
There are a number of clinical situations where it would be ill-advised to perform a total ankle replacement including:
Previous infection: a previous deep infection around the ankle will result in a high likelihood that the ankle replacement will become infected which is a major complication.
Neuropathy: Patients that do not have normal sensation in their feet and ankles will not do well in the long run with a total ankle replacement because the long term success of a joint replacement requires intact proprioception of the joint that is being replaced. Proprioception is the brains ability to sense what is happening to the joint at any point in time and make the necessary muscle contractions to ensure the joint is not excessively stressed.
Severe deformity: For an ankle replacement to work well over a long period of time it has to be well-balanced. Essentially the ankle prosthesis must be loaded evenly. In individuals with severe deformities achieving this type of even balancing becomes difficult or impossible.
Advanced avascular necrosis (AVN): Avascular necrosis of bone means that a section of bone has lost its blood supply. Loss of blood supply to part of the lower bone of the ankle joint (the talus) can occur and may lead to significant ankle arthritis. In these patients performing a total ankle replacement is not a good idea as the ankle replacement needs to be placed onto living bone. This is so that the bone can grow into the prosthesis, and so that the bone will have a good chance of remaining strong and solid enough to support the weight going through the prosthesis in the years ahead.
Potential Complications
These include the potential complications that can occur with any surgery such as:
There are some specific complications that can occur with total ankle replacement including:
Deep Infection of the Prosthesis
The deep wound infection rate in patients undergoing Total Ankle Replacement is not necessarily any higher than with other major ankle surgery. However, the significance of a deep infection is profound. A deep infection often requires removal of the prosthesis in order to eradicate the infection. The deep infection rate in patients undergoing a first time ankle replacement is approximately 1-3%.
Major Wound Breakdown
Most total ankle replacements are inserted through an incision in the front of the ankle. This area of skin and tissue in the front of the ankle has a somewhat tenuous blood supply. It is supplied by one main artery, whereas most other areas of the body are supplied by two or more major arteries. While wound healing problems are not frequent, proper surgical technique is required to minimize risks. Often, this requires immobilizing the ankle for a few weeks to improve the chances of successful wound healing. In some patients, an area of wound breakdown or a failure to heal the surgical incision can occur. A wound healing issue in this area can be a difficult and potentially devastating complication because the failure to obtain adequate wound healing can lead to a deep infection involving the prosthesis.
Tibial Nerve Injury
There is a chance of an injury to the nerves that surround the ankle joint, including the tibial nerve. A nerve injury is not likely, but can occur when the ankle joint is prepared to receive the ankle prosthesis.
Failure of the Ankle Replacement over time
All joint replacements will eventually fail if the patient uses the joint enough, and lives long enough. There are a variety of ways that joint replacements can fail, each of which lead to pain and dysfunction. Perhaps the most common mode of failure of a joint replacement is from shifting of the prosthesis. This can occur, often after many years, when the supporting bone becomes weak from repetitive loading or osteolysis. Osteolysis is the breakdown of the bone around the prosthesis usually resulting from a reaction of the immune system to very small particles of the polyethylene section of the prosthesis.
Total ankle replacements historically have failed earlier, and at a substantially higher rate, when compared to knee and hip replacements. For example, studies have suggested that certain hip replacements have good or excellent results in over 90% of patients after 18 years. In knee replacements, the figures are close to 90% success after an average of 15 years. However, in ankle replacements, the best prospective study suggests that 85-90% of patients have a successful result after 10 years – not bad, but nowhere near as successful as knee and hip replacement surgery. However, newer studies suggest that if an ankle replacement is functioing well 2 years after surgery, there is a very high likelihood that it will last at least 10 years.
Ankle replacements fail at a higher rate because of a variety of factors related to the ankle joint itself. These include:
- the small joint surface area (half the size of the knee joint)
- high joint reactive forces during walking (2-4 x body weight, almost twice that of the knee joint)
- Uneven distribution of force across the tibial prosthesis
- The lower bone of the ankle (Talus) is relatively small and has a poor blood supply, providing a less than ideal base of support for the prosthesis.
- There are limits to how much bone can be removed from the ankle joint, and this limits the size of polyethylene that can be used. The smaller the polyethylene, the poorer the wear characteristics
- The relatively confined nature (many important structures nearby) of the ankle joint makes placing an ankle replacement technically challenging for the surgeon.
When an ankle joint fails, a revision surgery is necessary. Often the prosthesis can be replaced. However, there may be much less bone stock available around the ankle, so revision surgery is often substantially more difficult with results that are less predictable than the original operation. If the prosthesis cannot be replaced, the ankle joint is then fused. However, studies suggest that patients who have an ankle fusion after a failed ankle replacement may do less well than patients who have an ankle fusion as an initial procedure. Newer implant designs which minimize bone resection and implants designed for revision total ankle arthroplasty will hopefully improve results of revision surgery.
Outcomes
Total Ankle Arthroplasty is being performed with increased frequency for end stage ankle arthritis. It’s important to consider many factors when considering this as a surgical option. While both ankle arthrodesis (fusion) and ankle replacement have similar outcomes as far as patient satisfaction, gait is more normal after ankle arthroplasty. Proper surgical indications and technique, as well as correction of any associated foot deformity, is imperative to achieving good outcomes.
Previously edited by Robert Leland, MD, and Sam Dellenbaugh, MD
Edited January 12th 2024
sp 1/12/24