Achilles Tendon Repair
Indication
An Achilles tendon repair is often performed as the surgical treatment for a ruptured Achilles tendon.
Procedure
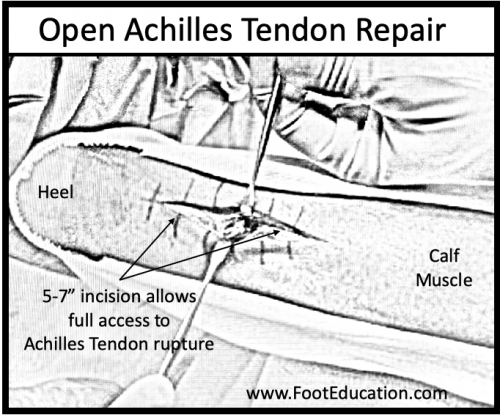
Open Achilles Tendon repair
An open Achilles tendon repair is performed through an approximately 3-inch incision running down the back of the ankle over the site of the Achilles tendon rupture. Each of the ruptured tendon ends are identified and sewn together with suture. The sutures from each end are tied to each other with the ankle pointing downwards so that the Achilles tendon is now under normal tension with the tendon ends touching each other. The wound is carefully closed and the ankle placed in a splint with the foot pointing downward (equinus) to protect both the wound and the repaired Achilles tendon as they begin to heal. (see Figure 1)
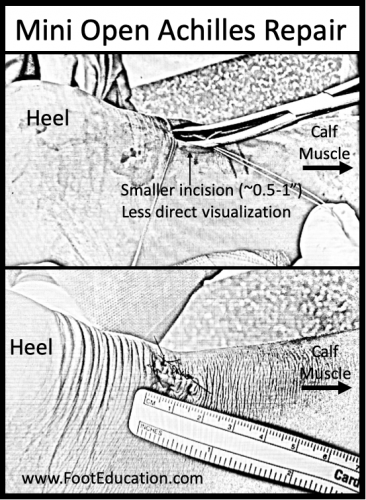
Mini-Open Incision
Minimally invasive approaches may also be used to repair the Achilles tendon and are often referred to as a “mini-open” technique (see Figure 2). In this procedure, a small incision measuring approximate half an inch is made over the Achilles rupture site. The Achilles tendon glides within a tendon sheath, and a special instrument is then used to pass sutures through the Achilles tendon and into this sheath using needles through the skin without making an actual incision running down the entire length of the repair, and the sutures are then pulled into the half-inch incision where they are tied. The “mini open” technique has the advantages of a smaller incision and a potentially lower rate of wound healing issues. However, a mini open repair has the disadvantage of less visualization of the ruptured tendon and a potentially higher rate of associated nerve injury.
Recovery
Typical Standard Recovery
Recovery from an Achilles tendon rupture and the associated surgical repair is a delicate balance between immobilization and movement. There needs to be enough immobilization early in the recovery to allow the wound and tendon to heal. Yet, recovery benefits from motion as soon as it is safe to do so. Gentle early motion (often starting 2-3 weeks post-surgery) aims to keep the tendon moving smoothly and the lower leg muscles firing so that soft-tissue scarring and muscle weakness (atrophy) is minimized. Historically, after Achilles tendon surgery patients would be placed in a cast with their toes pointing downwards for 6-8 weeks. More recently, studies have highlighted the importance of a more aggressive functional rehabilitation protocol in which the ankle is briefly immobilized to let the wound heal, but, thereafter, gradually increasing activity is allowed. This often entails gently moving the ankle to cause just a little bit of motion and tension at the healing tear site so that the tendon heals more strongly and with a less disorganized scar –but not too much tension so that it stretches or even re-tears the repair. Weight-bearing is gradually allowed in a specialized boot with multiple wedges under the heel so that the toes continue to point downwards and the repair isn’t stretched. After about 6 weeks these wedges are gradually removed so that the ankle is brought upwards in a controlled fashion over the course of a few weeks. Once out of the boot, progressive strengthening in a graduated manner is allowed. A return to full sport participation generally takes 6-12 months.
Potential General Complications
- Asymmetric Gait (leading to pain elsewhere)
- Deep Vein Thrombosis (Blood Clot)
- Pulmonary Embolism (PE)
- Scar Irritation
Potential Specific Complications
- Wound healing: While wound healing issues are a concern whenever surgery is performed on the foot or ankle, they are particularly concerning after an Achilles tendon repair because the tendon itself has relatively little soft-tissue coverage. Therefore, any type of wound healing problem can easily end up involving the tendon itself. For most patients, there is approximately a 2-5% chance of a wound-healing problem. Surgeons work hard to minimize these complications with careful soft tissue dissection and by trying to close the tendon sheath and skin separately to create a closure with multiple layers of protection, but the potential for a wound complication can never be eliminated –unless the Achilles rupture is treated non-surgically. The risk of a wound healing problem or infection following surgical repair of an Achilles tendon rupture is increased in patients who smoke or have diabetes. These risks are why many surgeons now recommend non-surgical management of Achilles tendon ruptures–especially considering potentially excellent clinical results can be achieved when an Achilles tendon rupture is treated non-surgically with a modern functional rehabilitation program.
- Infection: A deep infection following an Achilles tendon repair can be a devastating problem. Often, an infection will occur if there is an associated wound healing problem that allows bacteria from the outside world to reach the actual Achilles tendon. Treatment may require not only antibiotics, but potentially the removal of all suture materials and, in some instances, removal of the tendon itself. One may even need the participation of a plastic surgeon to get the skin to heal.
- Re-rupture of the Achilles tendon: The Achilles tendon can re-rupture after a repair. With surgery, re-rupture rates range from 2-5%. These tendon re-ruptures can occur at any time in the recovery process, but commonly occur 6-18 months (or longer) after the original surgery. Historically the rate of Achilles re-rupture was higher if one chose to treat the Achilles rupture without surgery (7-12%). Functional rehabilitation programs have lowered the re-rupture rate in this latter group, though research studies vary in whether they find that the re-rupture rate is similar with or without surgery in the setting of a functional rehabilitation protocol.
Previously edited by Vinod K. Panchbhavi, MD
Edited October 3rd, 2023
sp/10.3.23